If I told you that a plant-based compound, once used simply to treat skin, has the power to change how our cells handle life and death, would you believe me? Methoxsalen, pulled out of humble plants like Ammi majus, is more than an ingredient in a bottle. In labs and hospitals, it swings between healer and troublemaker, manipulating DNA repair and cell division like few other molecules can.
What Exactly Is Methoxsalen?
Let’s strip away the fancy chemical formulas for a second. Methoxsalen is a compound you’ll find lurking in certain plants, especially those in the parsley family. It’s also known as 8-methoxypsoralen, or just “psoralen” when folks are feeling lazy. Its molecular structure lets it slip into the double helix of DNA—kind of like a sneaky bookmark. For centuries, people have made teas or salves out of plants containing methoxsalen to ease skin issues like vitiligo and psoriasis. But it wasn’t until the mid-20th century that scientists discovered what methoxsalen really does: after you swallow it or rub it on your skin, and then get hit with ultraviolet (UV-A) light, it bonds with your DNA and changes how cells behave. This effect kicked off a treatment called PUVA (psoralen plus ultraviolet A). Fun fact: ancient Egyptians supposedly used sunlight and certain plants to manage skin problems, essentially inventing PUVA thousands of years before modern doctors gave it a name.
It’s the pairing of methoxsalen and UV-A that’s key. Alone, methoxsalen sits there almost harmlessly, but as soon as UV-A light shows up, those molecules go from wallflower to main event. The energy from UV-A pushes methoxsalen into action, letting it latch onto thymine bases—those are the building blocks—in DNA. Suddenly, methoxsalen isn’t just along for the ride, it’s driving the car.
How Methoxsalen Interferes with DNA
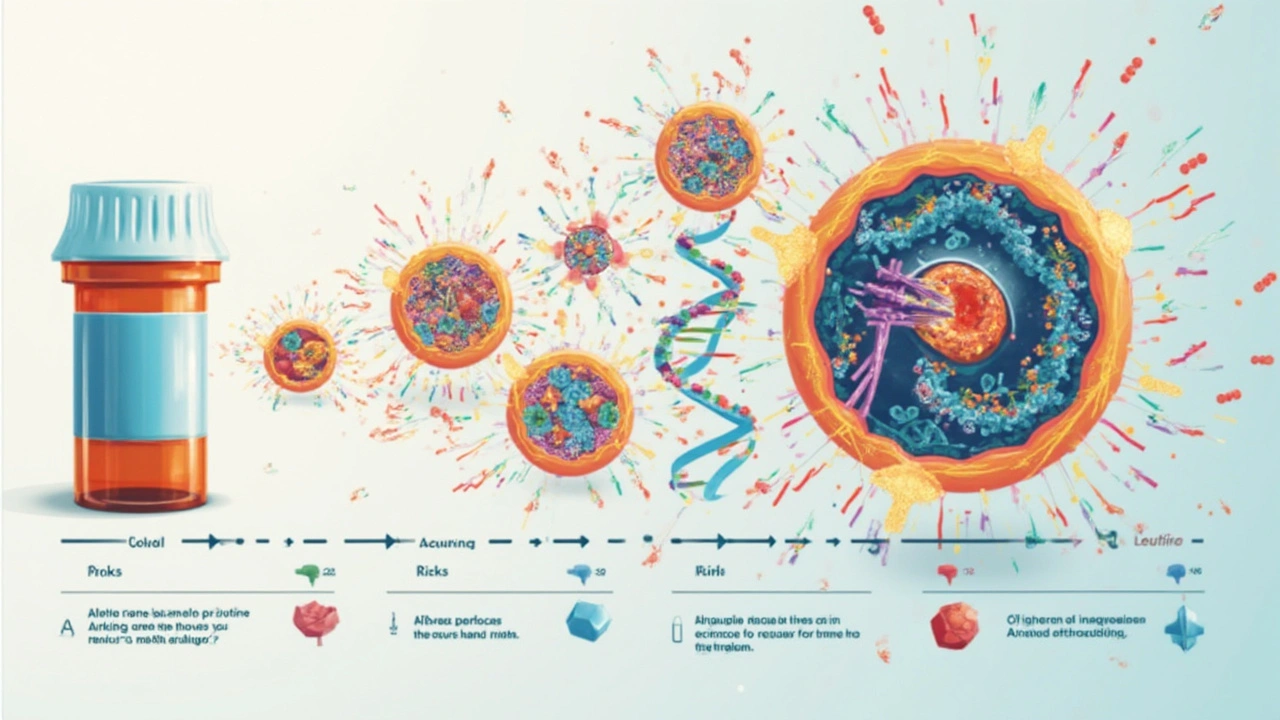
DNA repair might sound like something robots do in science fiction, but your cells are running this program all day long. And here’s where methoxsalen comes in like a plot twist. When methoxsalen interacts with DNA, especially under UV-A exposure, it forms what’s called a crosslink. Think of it as a zip tie connecting the two DNA strands together. Now, the DNA can’t unzip the way it normally would, which blocks replication and makes it hard for cells to divide. At first glance, this seems like bad news. But it’s actually a superpower in the right hands.
Here’s the trick: many skin conditions (and certain blood cancers) are caused by cells dividing out of control. By gumming up the works, methoxsalen stops this chaos, restoring some order. Back in the 1970s, researchers figured out that PUVA therapy—using methoxsalen with UV-A—could dramatically improve diseases like psoriasis. With one treatment, plaques could shrink, and the itching that kept people up at night would fade. Even more wild, after a few sessions, some people with vitiligo (where skin loses color) started to regain pigment.
Of course, the DNA crosslinks aren’t exactly gentle. These are serious modifications that your body recognizes as damage. The cell’s repair machinery (think: the molecular version of a pit crew) races to fix the broken parts. Nucleotide excision repair (NER) is one of the main repair systems that’s activated. When this works right, the damage is patched up before it can cause lasting trouble. But if repair crews are overwhelmed or the damage stacks up, the cell will panic and hit self-destruct: apoptosis. In cancer therapy, that’s exactly what doctors want.
Here’s a simple stat that drives it home: a study published in the Journal of Investigative Dermatology found that, after PUVA therapy, about 70% of psoriasis patients had major improvements within 4 to 6 weeks. But that improvement comes with a tradeoff. The DNA damage that helps control disease can also, over time, increase the risk of skin cancers if treatments aren’t managed carefully. That’s why doctors carefully monitor the total UV exposure and methoxsalen doses for each patient.
| Condition | Response Rate to PUVA Therapy | Main Risks |
|---|---|---|
| Psoriasis | ~70% major improvement | Skin cancer risk rises over years |
| Vitiligo | Partial pigment return in 40-60% of cases | Burning, skin aging |
| Cutaneous T-cell lymphoma | 45-80% respond well | Secondary skin cancers |

Cell Division: Speed Bumps and Dead Ends
Let’s break this down: your skin replaces itself about every four weeks, which means cell division is happening constantly. Normally, when DNA is copied during cell division, everything is super organized. But methoxsalen crosslinks are like tossing wrenches into the machinery. The DNA can’t unwind like it’s supposed to, and the enzymes that duplicate DNA get stuck. Suddenly, the cell can’t finish the process and stalls mid-division.
This effect is super helpful when we want to stop rogue cells—like psoriatic skin cells or cancer cells—from multiplying. Methoxsalen doesn’t just slow things down randomly; it’s pretty targeted, since only the cells exposed to PUVA become affected. Other cells, sheltering deep in the body or under layers of skin, don’t get hit as hard because less UV-A reaches them. That’s one reason PUVA is mostly used for surface conditions.
But there’s a catch: if normal cells get caught in the crossfire, or if treatments aren’t precisely managed, healthy cell growth can get stunted. This shows up as delayed wound healing or thin, fragile skin after too many treatments. Some people even notice their skin gets more sensitive to sunlight long after PUVA sessions end. That’s your DNA repair system working overtime to clean up the damage.
Scientists have tracked methoxsalen’s effects by using fluorescent markers on living cells and found that cells exposed to PUVA get stuck in the G2/M checkpoint—the point right before they divide. If they can’t fix their DNA in time, they self-destruct, a mechanism that keeps most of the damaged cells from turning into cancer. But if faulty cells slip through, that’s when side effects show up down the road. Staying ahead of this risk means limiting the total number of PUVA treatments to 200 or fewer over a patient’s lifetime, a rule backed up by multiple clinical guidelines.
Useful Tips and Safety Notes on Methoxsalen Use
If you ever end up in a dermatologist’s office and PUVA therapy comes up, a little know-how can save your skin—literally. Here are a few tips, backed by actual practice:
- Always wear protective eyewear during and after treatment. Methoxsalen makes the lens of your eye extra sensitive to UV, and skipping goggles can raise the risk of cataracts.
- Use sunscreen and cover up after each session. Methoxsalen sticks around in your body for several hours immediately after treatment, even if the therapy is over.
- Time your sessions. Morning and late afternoon sessions tend to lower the overall UV-A exposure your skin gets, reducing burn risk.
- Keep track of how many sessions you have had. Many clinics have logs, but it’s smart to track it yourself. Hit that 200-session mark, and you want to have a conversation with your doctor about alternatives.
- Digestive issues? Oral methoxsalen can upset your stomach. If you’re prone to tummy trouble, ask about topical versions or special coated tablets.
Doctors use a simple dosing rule: lower doses for people with lighter skin, and slightly higher doses for those with dark skin tones, since melanin absorbs some of the UV. Despite differences in risk, everyone gets regular skin checks for new moles or changes after a few months of therapy. This isn’t paranoia—long-term data collected over decades show a slight but real bump in skin cancer risk after many years of PUVA treatments. The tradeoff: for people with disabling skin conditions, the chance at clear, pain-free skin is worth it, especially with careful management.
Pregnant or breastfeeding? Methoxsalen isn’t recommended; the effects on fetal development or nursing babies aren’t clear—so doctors err on the side of caution. People with a history of lupus or other photosensitive diseases should tread carefully, since methoxsalen can flare these up.
Where Methoxsalen Research Is Heading
There’s always a plot twist in science, and methoxsalen is no different. While its best-known use is still in PUVA therapy, scientists have started digging into its abilities in genetics and cancer biology. Because methoxsalen’s DNA crosslinks are so specific, it’s being studied as a tool for editing genes or knocking out problem genes—in animal models, at least. The goal: learn more about how cells fix or deal with this type of damage, and maybe find new targets for cancer drugs that are less harsh but just as effective.
Some labs are messing around with modified versions of methoxsalen—changing its chemical structure slightly to control how deep it can travel into tissues, or how tightly it binds to DNA. This opens up options for new skin therapies, or for photodynamic treatments where precision is everything. You’ll even find methoxsalen in research kits, where it’s used to map out DNA-protein interactions and to test cell resilience to genetic insults.
Here’s something wild: some work is being done to deliver methoxsalen using nanoparticles, so it targets just cancerous or infected cells, sparing healthy ones. It’s still early days, but animal studies from universities in Europe and Asia show promise. If these experiments hold up, we could see PUVA-style treatments for internal diseases (not just the stuff you slap on your skin).
There’s also a ton of research looking at the limits of DNA repair. Every cell has its own “budget” for fixing damages. Methoxsalen is helping scientists figure out those limits: how much DNA can a cell fix before it gives up? If we can understand this budget, maybe we can design better, more targeted treatments for everything from rare skin disorders to stubborn tumors. Until then, methoxsalen remains a unique tool—half healer, half disruptor, with no signs of being replaced anytime soon.


akash chaudhary
July 18, 2025 AT 16:50First of all, let's get one thing straight — methoxsalen is not some magical potion that fixes everything in DNA repair without complications. It's a highly reactive compound, known mostly for its use in PUVA therapy for skin conditions like psoriasis. The article glosses over important details about the risks associated with its interaction with DNA, including the potential for mutagenesis and carcinogenesis if misused.
Honestly, any discussion about such a potent molecule should emphasize safety and the biochemical pathways involved. Methoxsalen intercalates with DNA, and under UV-A radiation, it forms cross-links that inhibit replication, which might be good for therapy but a double-edged sword in other contexts.
So yeah, while understanding its influence on cell division is fascinating, it's crucial not to oversimplify the implications. Readers need a clear understanding of its dual nature, therapeutic use, and risks rather than a watered-down explanation.
Rin Jan
July 18, 2025 AT 18:30Okay, okay, lemme dive in here a bit, cause this whole methoxsalen and DNA interaction thing? It's pretty wild, and honestly, people don't talk enough about how much these compounds mess with our cells on a deep, fundamental level.
I see the article is trying to keep it simple, but honestly, we need more awareness about how these drugs can sometimes interfere with natural cell processes beyond just repairing DNA. Like how it might impact long-term cell health and could potentially cause side effects that aren’t fully predictable.
It puzzles me how some folks take these treatments for granted, thinking it’s all safe and sound, when in reality, it's a delicate game of biochemical chess inside our bodies. The beauty and danger of methoxsalen both exist in those microscopic reactions that we barely understand. It's powerful stuff, and the article barely scratches the surface.
Adele Joablife
July 18, 2025 AT 20:10Honestly, methoxsalen has always been a topic that intrigues me. While I appreciate the article breaking down the basics, I’d love to see more about the ethical considerations of using such compounds, especially relating to treatment side effects.
There's a balance between innovation in medicine and knowing when the risks might outweigh the benefits. For instance, with methoxsalen’s ability to modify DNA under UV light, are we always fully aware of the long-term implications for patients? It's not just about how it works, but also about who it works for and if the existing protocols ensure patient safety.
The science is fascinating, but so is the responsibility that comes along with wielding it.
kenneth strachan
July 18, 2025 AT 21:50Oh, come on folks, can we just chill a bit with the fearmongering? Methoxsalen has been around for decades and used responsibly by professionals. I get that it’s this hefty chemical doing its DNA thing, but come on, it’s not like it's some villain from a sci-fi movie trying to mutate people left and right.
The article does a fine job breaking down a complex topic without going all medical textbook on us. Sometimes, it’s nice just to appreciate the cool chemistry happening inside our cells without immediately jumping to 'this must be dangerous!'.
Science needs to be understood, not feared. So yeah, I’m here to say let’s enjoy learning about methoxsalen for what it is — a tool, a fascinating one at that.
Mandy Mehalko
July 18, 2025 AT 23:30I'm really glad someone wrote something this clear and straightforward about methoxsalen. It’s not always easy to find info that’s both accessible and informative. I think getting the word out about how it works helps people understand treatments more and maybe even reduce anxiety about them.
Yes, the compound has risks, but science and medicine always have a balance of risks and benefits, right? Articles like this help people who might hear about methoxsalen in their treatment plans get a better grasp, so they don’t freak out when they hear about DNA stuff.
Hope to see more breakdowns like this that make complex topics approachable!
Tim Giles
July 19, 2025 AT 01:10Methoxsalen's mechanism of action, particularly its ability to intercalate into DNA and form covalent bonds after UV activation, reflects a fascinating convergence of chemistry and biology. This interaction has been explored in both therapeutic and experimental contexts. While the article provides a basic introduction, I think the nuances of how methoxsalen induces crosslinking between DNA strands which subsequently inhibits DNA synthesis and triggers repair pathways could be expanded upon.
The dual nature of its effects — therapeutic in controlled doses and environments versus potential genotoxicity — deserves detailed discussion, especially for readers interested in molecular pharmacology or cellular biology.
Moreover, exploring its historical development and variations in clinical protocols could provide a comprehensive perspective on its impact on modern medicine.
Peter Jones
July 19, 2025 AT 02:50This topic really highlights the complexity of using chemical agents to influence biological systems. Methoxsalen, acting as a photosensitizer, plays a unique role where light and chemical exposure combine for therapeutic gain.
I appreciate how the article brings out the practical applications while not diving too deep into jargon that might overwhelm general readers. Understanding how methoxsalen affects cell division through DNA cross-linking and repairs broadens the appreciation for targeted treatment strategies, particularly in dermatology and oncology.
It’s always a fine line between explaining enough to inform and not so much to confuse, and here I think the article strikes a reasonable balance.
Gerard Parker
July 19, 2025 AT 04:30I'm compelled to highlight some critical aspects that the article didn’t extensively cover. Methoxsalen has been utilized extensively in PUVA therapy, but there are cultural and societal dimensions linked to its application. For example, accessibility to such treatments varies internationally and raises questions about equity in healthcare.
Furthermore, the compound’s mutagenic potential necessitates strict regulation and monitoring which isn’t always uniformly applied worldwide. The risks of skin cancer induction in long-term PUVA patients underline the importance of ongoing research and ethical clinical practices.
Therefore, while the article is informative, a deeper analysis of methoxsalen’s role amidst socio-medical realities would enhance the discussion significantly.
Michelle Abbott
July 19, 2025 AT 06:10Reading this post, I can’t help but think the article is stuck trying to please both lay readers and professionals, but ends up doing neither convincingly. The language is occasionally vague and overly simplistic when the science deserves more precision.
For instance, terms like “influence on DNA repair” and “fundamental cell processes” are tossed around without much detail or reference. There’s a nebulous feel that leaves readers hanging; it neither educates thoroughly nor satisfies those looking for scientific depth.
It's a missed opportunity to weigh in on controversial aspects like off-label uses or the biochemical pathways involved. I wish the article took a stronger stance or at least provided more concrete substantiation.
Heather Jackson
July 19, 2025 AT 07:50As someone from Canada who appreciates a good scientific read that doesn't feel too heavy, I found this article quite digestible. It balances drama and facts just enough to keep me interested, especially when it explains how methoxsalen can impact something as delicate as DNA and cell division.
Sometimes science articles get really dense, but this one kept me engaged. I think the focus on both the medical applications and the basic cellular interactions makes it useful for a wide audience. I’d be curious to know more about ongoing research though — like new derivatives of methoxsalen or safer ways to use it.
Bryan Kopp
July 19, 2025 AT 09:30While I am often reluctant to jump on the bandwagon of praising anything that tinkers with DNA considering my perspective on American overreliance on pharmaceuticals, I must admit that methoxsalen in controlled medical settings reflects our progress in precision medicine.
The ability to harness a compound that can cross-link DNA to treat ailments shows the potential of modern science when balanced with responsibility. However, caution remains paramount, and such knowledge must always be coupled with stringent regulations and ethical considerations to avoid misuse.
This article, in its own way, contributes to spreading awareness — but let’s never forget the bigger picture of healthcare systems and their impacts on society.