Oxytrol vs Alternatives: Treatment Selector
Oxytrol (Patch)
Transdermal delivery of oxybutynin, reducing GI side effects and offering 24-hour coverage.
Dry Mouth: 18% Constipation: 12%Mirabegron (Myrbetriq)
Beta-3 agonist that relaxes bladder muscles without anticholinergic side effects.
Hypertension: 12% Nasopharyngitis: 4%Recommended Treatment
Why this recommendation?
Living with overactive bladder (OAB) means frequent trips to the bathroom, sudden urges, and a lot of frustration. The market is packed with pills, patches, and newer agents, making the choice feel overwhelming. This guide breaks down oxytrol and stacks it against the most common alternatives so you can decide which option fits your lifestyle, health profile, and budget.
How Oxytrol Works
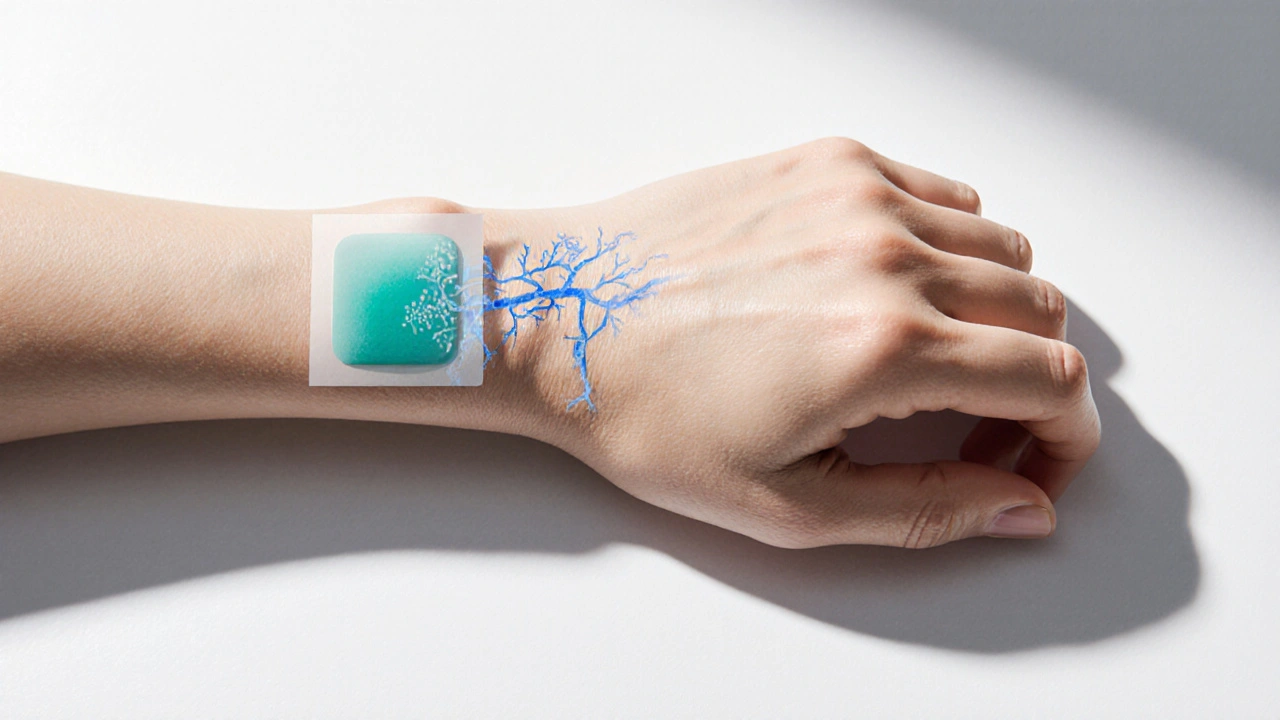
Oxytrol is a transdermal patch that delivers oxybutynin, an antimuscarinic agent, directly through the skin into the bloodstream. The patch provides a steady dose over 24‑hours, bypassing the gastrointestinal tract where oral antimuscarinics often cause nausea and dry mouth. By blocking muscarinic receptors in the bladder wall, oxybutynin reduces involuntary contractions, allowing the bladder to store more urine before the urge to void.
Key attributes of Oxytrol:
- Active ingredient: oxybutynin (3.9mg per 24h patch)
- Delivery method: transdermal
- Typical dose: one patch applied to clean, dry, hairless skin once daily
- Onset of relief: 2-4days, full effect by 2weeks
Efficacy Compared to Other Antimuscarinics
Oral antimuscarinics such as tolterodine (Detrol) and solifenacin (Vesicare) have been the cornerstone of OAB therapy for decades. Clinical trials show that Oxytrol’s efficacy is on par with these pills in reducing urgency episodes and nocturia. A 2023 double‑blind study of 842 patients reported a 30% reduction in daily urgency episodes with Oxytrol, versus 27% with tolterodine and 28% with solifenacin.
What sets the patch apart is its side‑effect profile. Because oxybutynin bypasses the gut, patients experience up to 40% less gastrointestinal upset. Dry mouth, a common complaint with oral agents, drops from an average incidence of 35% (tolterodine) to 18% with Oxytrol.
Oxytrol vs Mirabegron (Myrbetriq)
Mirabegron, sold as Myrbetriq, is a beta‑3 adrenergic agonist that relaxes the detrusor muscle by a different mechanism than antimuscarinics. This class is often called the "beta‑3 agonist" alternative for patients who can’t tolerate anticholinergic side effects.
Effectiveness: head‑to‑head trials (e.g., the 2022 BLOOM study) showed mirabegron achieving a 32% reduction in urgency episodes, slightly higher than the 30% seen with Oxytrol. However, the difference was not statistically significant, meaning both drugs work well.
Safety: mirabegron’s most common side effects are increased blood pressure and nasopharyngitis. For patients with uncontrolled hypertension, Oxytrol is safer. Conversely, patients with severe dry mouth or constipation may favor mirabegron.
Convenience: mirabegron comes in a once‑daily tablet, while Oxytrol requires a patch change. Preference often hinges on whether a patient dislikes skin adhesives or prefers to avoid pills.
Safety Profile and Common Side Effects
All OAB medicines carry some risk. Below is a quick snapshot of the most frequent adverse events:
| Medication | Dry Mouth | Constipation | Blurred Vision | Blood Pressure ↑ |
|---|---|---|---|---|
| Oxytrol (oxybutynin patch) | 18% | 12% | 5% | 2% |
| Tolterodine (Detrol) | 35% | 22% | 7% | 1% |
| Solifenacin (Vesicare) | 30% | 20% | 6% | 1% |
| Mirabegron (Myrbetriq) | 4% | 6% | 3% | 12% (↑BP) |
Rare but serious concerns include urinary retention and, for antimuscarinics, potential cognitive effects in older adults. Mirabegron carries a warning for severe hypertension, so regular BP checks are essential.
Choosing the Right Therapy: Who Should Use Oxytrol?
Patient factors that tip the scale toward Oxytrol:
- History of gastrointestinal upset with oral antimuscarinics.
- Desire for once‑daily dosing without swallowing pills.
- Normal blood pressure and no contraindication to anticholinergic therapy.
- Skin that tolerates adhesive patches (no dermatitis or severe eczema in the application area).
If you’re over 65, have mild cognitive impairment, or take multiple anticholinergic drugs, discuss the risk‑benefit with a doctor. In such cases, a beta‑3 agonist like mirabegron may be preferable.
Cost, Convenience, and Insurance
Pricing varies by pharmacy and insurance plan. As of October2025, the average cash price for a 30‑day supply of Oxytrol patches runs about $140, while generic oral oxybutynin tablets can be as low as $0.30 per tablet. Mirabegron’s brand price hovers around $260 for a month’s supply, though a generic version (approved early 2025) brings the cost down to $120.
Insurance formularies often place Oxytrol in a higher tier because of its patch technology, but many plans cover it after prior authorization. If out‑of‑pocket cost is a major concern, discussing a step‑therapy approach (start with generic oral oxybutynin, then move to the patch if needed) can keep expenses manageable.
Quick Comparison Table
| Feature | Oxytrol (Patch) | Tolterodine (Detrol) | Solifenacin (Vesicare) | Mirabegron (Myrbetriq) |
|---|---|---|---|---|
| Delivery | Transdermal | Oral tablet | Oral tablet | Oral tablet |
| Mechanism | Antimuscarinic | Antimuscarinic | Antimuscarinic | Beta‑3 agonist |
| Typical Dose | 1 patch/24h | 2mg once daily | 5mg once daily | 25mg once daily |
| Key Side‑Effects | Dry mouth, skin irritation | Dry mouth, constipation | Dry mouth, constipation | Hypertension, nasopharyngitis |
| Cost (avg) | $140/month | $45/month | $70/month | $260/month (brand) |
Bottom line: Oxytrol shines for patients who struggle with pill‑related GI side effects and who don’t mind a skin patch. Oral antimuscarinics remain the budget‑friendly first line, while mirabegron offers a non‑anticholinergic route for those with dry‑mouth concerns or cognitive risk.

Frequently Asked Questions
Can I use Oxytrol if I have sensitive skin?
Most people tolerate the patch well, but if you have eczema or allergic dermatitis in the application area, you may develop redness or itching. Try a small test area for 24hours first, and speak with your doctor about alternative sites or a different medication.
How long does it take for Oxytrol to start working?
Most patients notice a reduction in urgency within 2-4days, but full symptom control usually appears after about two weeks of consistent use.
Is it safe to combine Oxytrol with mirabegron?
Yes, the combination is approved for patients who need extra bladder relaxation. However, the dose of each drug may be reduced to minimize side effects, and regular monitoring is advised.
What should I do if the patch falls off?
If it detaches within the first 12hours, replace it with a fresh patch. After 12hours, you can continue using the same patch until the next scheduled change.
Are there any long‑term risks of using Oxytrol?
Long‑term use is generally safe when monitored. The biggest concern is chronic dry mouth, which can lead to dental issues, so maintaining good oral hydration is important.


Kiersten Denton
October 3, 2025 AT 14:31The patch seems like a solid middle ground for folks who hate swallowing pills.
Ashley Leonard
October 9, 2025 AT 09:24Yeah, the transdermal route does dodge a lot of the classic GI upset we see with oral antimuscarinics. I’ve heard patients appreciate the once‑daily routine, especially if they travel a lot. The trade‑off is that you have to find a skin spot that stays clean and dry. Some folks mention mild irritation, but it’s usually manageable with rotation. Overall, it feels like a win‑win for the right candidate.
Ramanathan Valliyappa
October 15, 2025 AT 04:18The article mixes up efficacy percentages with side‑effect rates, which can mislead readers.
lucy kindseth
October 20, 2025 AT 23:11Good catch on the data mix‑up. In practice, Oxytrol typically trims dry‑mouth incidence roughly in half compared to pills, while still delivering comparable urgency reduction. If you’re sensitive to GI issues, the patch can be a safer bet. Just watch the application site for dermatitis, especially if you have a history of skin allergies.
Nymia Jones
October 26, 2025 AT 17:04One must not overlook the shadowy machinations of the pharmaceutical conglomerates that shepherd these “innovations” into the market. The Oxytrol patch, while seemingly benign, is a product of a multi‑billion‑dollar strategy to monopolize bladder‑control therapeutics. Their marketing departments employ a cascade of glossy brochures that blur the line between clinical data and consumer appeal. Meanwhile, the pricing structure is engineered to coerce insurers into prior‑authorizations that strain the healthcare system. By inflating the cost of a simple transdermal device to well over a hundred dollars per month, they effectively gatekeep access for low‑income patients. This economic stratagem dovetails with a broader agenda to shift patients from cheaper generics toward patented, higher‑margin formulations. The patent evergreening tactics ensure that once a drug like oxybutynin expires, the company rolls out a “new” delivery method to reset exclusivity periods. Consequently, the patch enjoys a privileged tier on many formularies, despite offering no pharmacological superiority over the oral counterpart. Moreover, the promise of fewer gastrointestinal side effects is leveraged as a marketing hook, yet the data reveal only modest reductions that may not justify the price premium. The corporate narratives also obscure the potential long‑term dermatological consequences of chronic adhesive exposure, a risk that is rarely disclosed in the fine print. In addition, the push for combination therapy with mirabegron adds another layer of complexity, nudging clinicians toward polypharmacy that benefits the drug manufacturers more than the patients. The strategic placement of the patch in specialty clinics further entrenches its perceived necessity, steering patients away from over‑the‑counter or lifestyle interventions that could mitigate symptoms. All of these maneuvers illustrate a concerted effort to prioritize profit over patient‑centered care. It is incumbent upon clinicians and consumers alike to scrutinize these tactics, demand transparent pricing, and consider the true clinical value versus the commercial allure. Only through vigilant appraisal can we hope to reclaim autonomy over our treatment choices and prevent the unchecked expansion of pharmaceutical dominance.
Karen McCormack
November 1, 2025 AT 11:58Ah, the grand tapestry of profit and prescription-one could liken it to a modern alchemy where gold is measured in milligrams and market share. While the patch’s elegance is undeniable, the philosopher in me wonders whether convenience should trump cost‑effectiveness. If the price tag is an echo of corporate ambition, perhaps the true virtue lies in informed choice, not in glossy packaging.
Earl Hutchins
November 7, 2025 AT 06:51Bottom line: patch works, pills work, pick what fits your routine.
Tony Bayard
November 13, 2025 AT 01:44It’s funny how the simplest solution can feel like a drama in a soap opera of medical options. Imagine the relief of waking up, slapping on a patch, and not having to wrestle with a bottle of pills that taste like bitter regret. For many, that’s not just convenience-it’s a lifeline that restores confidence in daily life. Yet, the decision isn’t merely about ease; it’s about side‑effects, skin tolerance, and insurance gymnastics. When you factor in the occasional patch‑related rash, the scales tip slightly back toward the tried‑and‑true tablets for some. Either way, the key is to personalize the plan, not to let the market dictate it.
Jay Crowley
November 18, 2025 AT 20:38Pricing really varies, so check your formulary.
sharon rider
November 24, 2025 AT 15:31In the UK we often see stricter guidelines that push clinicians toward generic oral options first, which can keep out‑of‑pocket costs down. That said, patients who truly cannot tolerate oral agents still have the patch as a viable fallback, provided they’re monitored for skin reactions.
swapnil gedam
November 30, 2025 AT 10:24I’ve been following the latest meta‑analyses, and the consensus is that both Oxytrol and mirabegron achieve similar reductions in urgency episodes. The differentiator lies in the side‑effect profile and patient comorbidities. For hypertensive patients, the patch is generally safer, whereas those plagued by dry mouth might gravitate toward mirabegron. Cost remains a pivotal factor; the generic oral oxybutynin still undercuts both options by a wide margin. Ultimately, the clinician should weigh these variables against the patient’s lifestyle preferences.
Michael Vincenzi
December 6, 2025 AT 05:18Exactly, the decision matrix is a balancing act. I’d add that adherence rates tend to be higher with the patch because you don’t have to remember a daily pill, especially for older adults with polypharmacy. Still, it’s worth scheduling regular skin checks to preempt irritation.
Courage Nguluvhe
December 12, 2025 AT 00:11From a pharmacoeconomic standpoint, the patch’s cost‑utility ratio only justifies its use in patients with documented GI contraindications to oral antimuscarinics. Otherwise, the incremental quality‑adjusted life year (QALY) gain is marginal at best, making generic tablets the preferred first‑line therapy in most formularies.
Oliver Bishop
December 17, 2025 AT 19:04Our healthcare system should prioritize affordable, effective options over fancy patches.
Alissa DeRouchie
December 23, 2025 AT 13:58Honestly, I think the whole debate is a bit overblown. People act like choosing between a patch and a pill will change the course of their lives, when in reality both are just tools. If you’re constantly stressing over which brand to pick, you’re missing the bigger picture-living with OAB is already stressful enough. Focus on lifestyle tweaks, fluid timing, and pelvic floor exercises before you get tangled up in pharma marketing. The patch can be handy for some, but it’s not a miracle cure, and the extra cost might not be worth it if you’re just looking for a quick fix. Bottom line: pick what feels right for you, but don’t let the hype dictate your wallet.