ACE Inhibitor and ARB Interaction Checker
Your Medication Status
Select your current medication situation to see what the evidence says
What to Do Next
Please select your medication status to see recommendations
Key Facts About Combination Therapy
Why Combining Is Dangerous
- Hyperkalemia risk 2x increase
- Acute kidney injury 1.8x increase
- Need for dialysis >2x increase
- Serious side effects 27% higher
When your doctor prescribes an ACE inhibitor or an ARB for high blood pressure or kidney protection, you might assume they’re just two versions of the same thing. But they’re not. And mixing them? That’s where things get risky.
How ACE Inhibitors and ARBs Actually Work
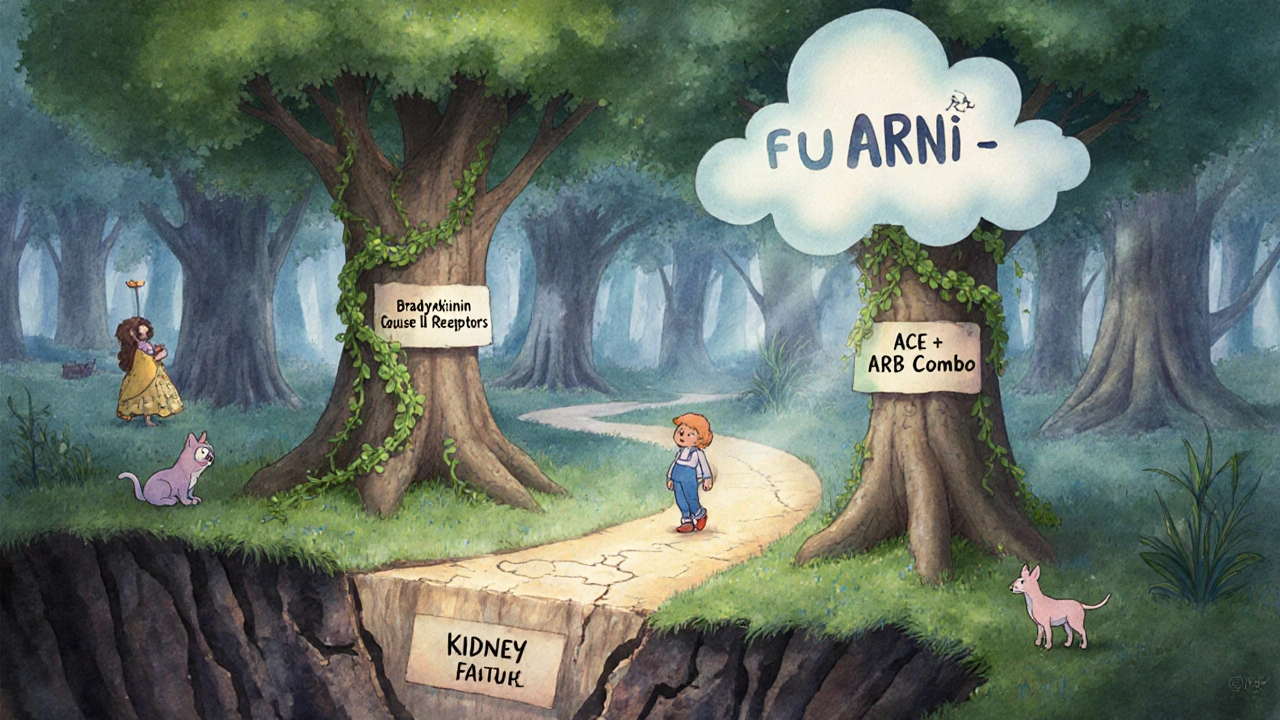
Both ACE inhibitors and ARBs target the same system in your body-the renin-angiotensin system-but they hit different buttons. ACE inhibitors, like lisinopril and enalapril, stop your body from making angiotensin II, a chemical that tightens blood vessels and raises blood pressure. ARBs, such as losartan and valsartan, let your body make angiotensin II but block it from binding to receptors that cause blood pressure to spike.
This small difference matters. ACE inhibitors cause bradykinin to build up, which is why about 1 in 10 people on these drugs get a dry, annoying cough. ARBs don’t do that. That’s why many people switch from an ACE inhibitor to an ARB-not because the first one didn’t work, but because the cough was unbearable.
Here’s another twist: ACE inhibitors lower angiotensin II levels at first, but after six months, your body finds a workaround. About two-thirds of patients see angiotensin II levels bounce back up to 25-30% of normal. That’s called ‘partial escape.’ ARBs don’t have this issue because they’re blocking the receptor, not the enzyme. So even if angiotensin II levels rise, it can’t do damage.
Why Mixing Them Is Dangerous
It sounds logical-take both to block the system twice as hard. But that’s not how it works. In 2008, the ONTARGET trial gave over 25,000 high-risk patients either ramipril (an ACE inhibitor), telmisartan (an ARB), or both. The results were shocking. The combo lowered blood pressure by a few extra points and cut proteinuria a bit more. But it doubled the risk of dangerously high potassium levels and made acute kidney injury 1.8 times more likely. Worse, it increased the chance of needing dialysis by more than double.
That’s not an outlier. The VA NEPHRON-D trial in 2018 looked at people with diabetic kidney disease. Those on both drugs had a 27% higher rate of serious side effects-like hospitalizations for high potassium or kidney failure-with zero improvement in heart attacks, strokes, or death. The FDA and major heart associations now say: don’t combine them. Not unless you’re in a clinical trial.
Real-world data backs this up. A 2023 survey of 317 primary care doctors found that 89% had stopped prescribing the combo after seeing the data. One nephrologist in Massachusetts reported discontinuing the combination in 87% of her patients with diabetic kidney disease because of spikes in potassium or drops in kidney function.
Who Might Still Get Both? (And Why It’s Rare)
There’s one tiny gray area. A small group of doctors, like Dr. Srinivasan Beddhu from the University of Utah, say that in rare cases-like non-diabetic patients with proteinuria over 1 gram per day who’ve maxed out an ACE inhibitor-a carefully monitored ARB might help. But even then, it’s not a first choice.
These patients need weekly blood tests for potassium and creatinine. They’re watched like hawks. Most clinics won’t even try it. The National Kidney Foundation’s patient forum has only 12 documented cases where this combo helped reduce proteinuria by 40-60%. All required intense monitoring. For every one success, there are dozens of hospitalizations.
There’s no benefit for heart failure, stroke prevention, or survival. The risks far outweigh any small kidney benefit. That’s why most guidelines call it a no-go.
Side Effects You Can’t Ignore
Even when used alone, these drugs have risks. Both can raise potassium levels by 0.3-0.5 mmol/L on average. In older adults or people with kidney disease, that’s enough to cause heart rhythm problems. About 5-10% of high-risk patients develop acute kidney injury within the first few weeks of starting either drug.
Angioedema-swelling of the face, lips, or throat-is rare but life-threatening. It happens in 0.1-0.7% of ACE inhibitor users. For ARBs? Just 0.1-0.2%. That’s why if you’ve had angioedema on an ACE inhibitor, you’re usually switched to an ARB. But even then, there’s still a small risk.
And here’s something few patients know: ARBs were recalled in 2018-2020 because of cancer-causing nitrosamine impurities. Valsartan, losartan, and irbesartan batches were pulled. Most of those issues are fixed now, but it’s a reminder that these drugs aren’t risk-free-even when used correctly.
Switching Between Them? Do It Right
If you’re switching from an ACE inhibitor to an ARB (or vice versa), don’t just stop one and start the other the next day. There’s a reason the 2023 ACC guidelines recommend a 4-week washout period. Why? Because even after you stop an ACE inhibitor, its effects linger. Starting an ARB too soon can cause additive drops in blood pressure or kidney function.
But here’s the problem: only 42% of doctors follow this rule. Many patients are switched cold turkey. That’s why some end up dizzy, fainting, or with a sudden drop in kidney function. Always ask your doctor: ‘Do I need to wait before starting the new one?’
What to Do Instead of Combining Them
If your blood pressure isn’t controlled on one drug, don’t add another RAS blocker. Add something safer.
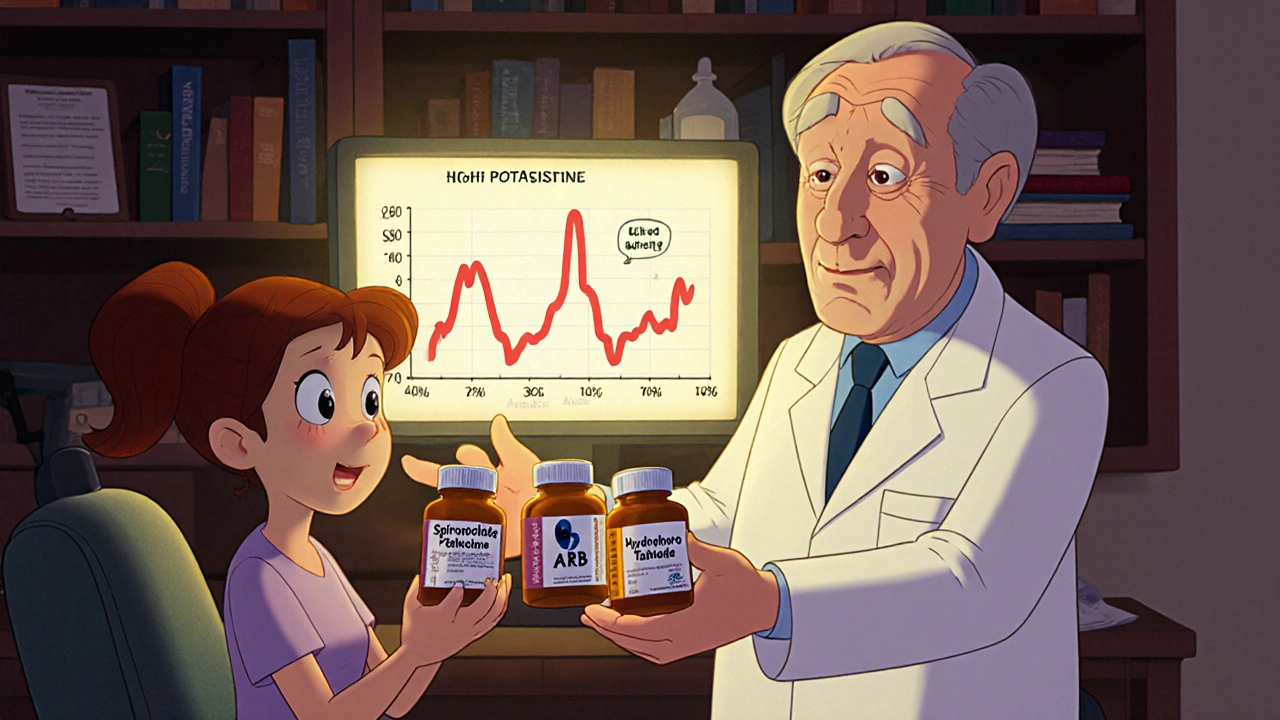
For example, adding a low-dose spironolactone (12.5 mg daily) can cut proteinuria by 30-40% without the same risks as an ARB-ACE combo. It’s a mineralocorticoid receptor antagonist, so it works differently. It’s also used in heart failure and has proven survival benefits.
Another option? Thiazide diuretics like hydrochlorothiazide. They’re cheap, effective, and don’t raise potassium as much as ARBs or ACE inhibitors. Or try a calcium channel blocker like amlodipine. These are the go-to second-line choices for a reason.
Monitoring Is Non-Negotiable
Whether you’re on one or the other, you need blood tests. Not every year. Not every six months. At least 1-2 weeks after starting or changing the dose, then every 3 months after that. Check potassium and creatinine. That’s it. Two simple tests.
If your potassium climbs above 5.5 mmol/L or your creatinine rises by more than 30%, your doctor should pause the medication. Not just adjust the dose. Pause. Reassess. This isn’t optional. It’s life-saving.
Studies show that patients who get regular monitoring have 60% fewer hospitalizations for kidney or heart problems than those who don’t.
What’s Next? New Options Are Coming
The future isn’t in combining ACE inhibitors and ARBs. It’s in moving past them.
Drugs like ARNIs (angiotensin receptor-neprilysin inhibitors), such as sacubitril/valsartan, are now first-line for heart failure with reduced ejection fraction. They’ve outperformed ACE inhibitors in survival trials. And they don’t carry the same cough or angioedema risks.
There’s also a new trial running right now-the FINE-REWIND study-testing ultra-low doses of both an ACE inhibitor and ARB in diabetic kidney disease. Results won’t come until 2026. But even if they show benefit, it’ll be in a tiny, tightly controlled group. Not for general use.
By 2028, experts predict less than 1% of RAS blocker prescriptions will involve combining ACE inhibitors and ARBs. The market is shifting to safer, smarter options.
Bottom Line
ACE inhibitors and ARBs are powerful tools. But they’re not interchangeable, and they’re not meant to be stacked. The data is clear: combining them increases the risk of kidney failure, high potassium, and hospitalization-with no added benefit for survival or heart health.
If you’re on one and your blood pressure isn’t controlled, talk to your doctor about adding a diuretic, a calcium channel blocker, or spironolactone-not another RAS blocker.
If you’ve been switched from an ACE inhibitor to an ARB because of a cough, you made the right choice. But don’t go back.
And if someone tells you ‘it’s fine to take both’-ask them to show you the study that proves it’s safe. Chances are, they can’t.
Can I take an ACE inhibitor and an ARB together for better blood pressure control?
No. Combining ACE inhibitors and ARBs increases the risk of dangerous side effects like hyperkalemia (high potassium) and acute kidney injury without improving survival or reducing heart attacks or strokes. Major guidelines from the AHA, ACC, and ESC strongly advise against this combination outside of rare, closely monitored research settings.
Why do some people switch from ACE inhibitors to ARBs?
The most common reason is a persistent dry cough, which affects 10-15% of people on ACE inhibitors due to bradykinin buildup. ARBs don’t cause this side effect because they work differently-blocking angiotensin II receptors instead of stopping its production. Switching to an ARB often resolves the cough without losing blood pressure control.
Are ARBs safer than ACE inhibitors?
In terms of side effects, yes-ARBs have a better safety profile. They cause less cough (3-5% vs. 10-15%) and slightly lower rates of angioedema. However, both classes carry similar risks for high potassium and kidney injury. Neither is universally ‘safer’-the choice depends on your individual tolerance and medical history.
What should I do if my potassium levels rise on an ACE inhibitor or ARB?
If your potassium rises above 5.5 mmol/L or your kidney function declines by more than 30%, your doctor should pause the medication. Do not adjust the dose yourself. High potassium can cause dangerous heart rhythms. Your doctor may recommend dietary changes, a diuretic, or switching to a different class of blood pressure medication.
Is it safe to switch from an ACE inhibitor to an ARB right away?
No. Experts recommend a 4-week washout period between stopping an ACE inhibitor and starting an ARB to avoid additive effects on blood pressure and kidney function. However, many doctors skip this step. Always ask your provider if you need to wait and why.
What are the alternatives if I can’t take ACE inhibitors or ARBs?
If you can’t tolerate either drug, your doctor may prescribe a calcium channel blocker like amlodipine, a thiazide diuretic like hydrochlorothiazide, or a mineralocorticoid receptor antagonist like spironolactone. These are proven alternatives that don’t carry the same risks as combining ACE inhibitors and ARBs.


shreyas yashas
November 23, 2025 AT 19:09Been on lisinopril for 5 years. Cough was brutal. Switched to losartan and it’s like a new person. No cough, same BP control. Just don’t eat bananas like they’re candy anymore 😅
Laurie Sala
November 25, 2025 AT 17:35Wait… so you’re telling me… that doctors are actually… *not* supposed to… prescribe both?!?!?!?!?!?!?!? I thought this was the ‘super combo’! I’m so confused now… I feel like I’ve been lied to…
Matthew Mahar
November 26, 2025 AT 21:11My grandpa was on both for 3 months. Ended up in the ER with potassium at 6.8. He’s fine now, but they had to put him on a dialysis machine for a day. Don’t mess with this stuff. It’s not a game. 🙏
Suresh Ramaiyan
November 28, 2025 AT 01:54It’s funny how we treat medicine like a stackable power-up in a video game. You don’t combine fire and water to make a better flame-you just get steam. Same here. The body isn’t a machine you overclock. It’s a dance. You have to listen.
Ragini Sharma
November 29, 2025 AT 01:47so like… if i have diabetez and kidney issues and my doc says ‘try both’… am i just a guinea pig? 😭
Katy Bell
November 29, 2025 AT 12:35I had a friend who switched from lisinopril to valsartan because of the cough… and then found out her batch was recalled in 2019. She was terrified for months. Turns out it was a new lot, but still… the anxiety? Real. This stuff isn’t just pills. It’s emotional baggage.
Adrian Rios
November 30, 2025 AT 01:45Let’s be real-most primary care docs are drowning in patients and 20-minute appointments. They don’t have time to explain the nuance of partial escape or the 4-week washout period. So they do what’s easy: swap one for the other, no waiting. And patients? They just take it. No questions. Until they’re dizzy in the shower or their creatinine spikes. We need better systems, not just better guidelines. The system is broken, and we’re paying for it with our kidneys.
Linda Rosie
December 2, 2025 AT 01:42Combining ACE inhibitors and ARBs is contraindicated per current AHA/ACC/ESC guidelines. Risk of hyperkalemia and acute kidney injury significantly elevated. No mortality benefit observed. Alternatives include thiazides, CCBs, or spironolactone.
Lisa Detanna
December 2, 2025 AT 23:49As someone from a country where doctors still prescribe both because ‘it’s cheaper than new drugs’-I’ve seen the fallout. Elderly patients in rural clinics getting hospitalized for potassium spikes. We need global education. This isn’t just an American problem. It’s a global blind spot. And we’re not talking about it enough.
Vivian C Martinez
December 3, 2025 AT 23:23If you’re on one of these and your BP isn’t controlled, talk to your doctor about adding a diuretic or calcium channel blocker. These are proven, safer options. Don’t reach for the second RAS blocker. Your kidneys will thank you.
Casper van Hoof
December 4, 2025 AT 04:38The renin-angiotensin system is not a linear pathway-it is a recursive feedback loop, a biological echo chamber. To block one node is to invite compensation. To block two is to invite collapse. The body does not understand intention. It only responds to pressure. We mistake control for mastery. We are not engineers. We are guests.
Karla Morales
December 4, 2025 AT 17:16Just saw a patient today who was on both drugs for 8 months. Got dialysis last week. His wife said, ‘He just trusted his doctor.’ That’s not trust-that’s negligence. We need better patient education. Maybe a simple infographic in every prescription bottle? 📊🩺
John Mackaill
December 6, 2025 AT 04:41My cousin in London was switched from lisinopril to losartan after the cough. Then her GP added spironolactone for proteinuria. Her potassium stayed stable, kidney function improved. She’s been on it for 2 years. No hospital visits. This is what safe looks like. Not stacking. Layering with care.
Brandy Walley
December 8, 2025 AT 03:33so the whole time i thought i was being smart taking both… turns out i was just being a dumbass? wow. thanks for the reality check. now i feel dumb. but also relieved?
Adrian Rios
December 9, 2025 AT 18:08Actually, I’ve seen a few cases where a low-dose combo was used in non-diabetic proteinuria patients with no other options. But only after 3 months of failing everything else-and only with weekly labs. One guy’s proteinuria dropped 50%. But his potassium hit 5.8. He had to stop. It’s not impossible. It’s just not worth it for 99% of people. And that’s the problem-we hear the 1% success stories and forget the 99% disasters.