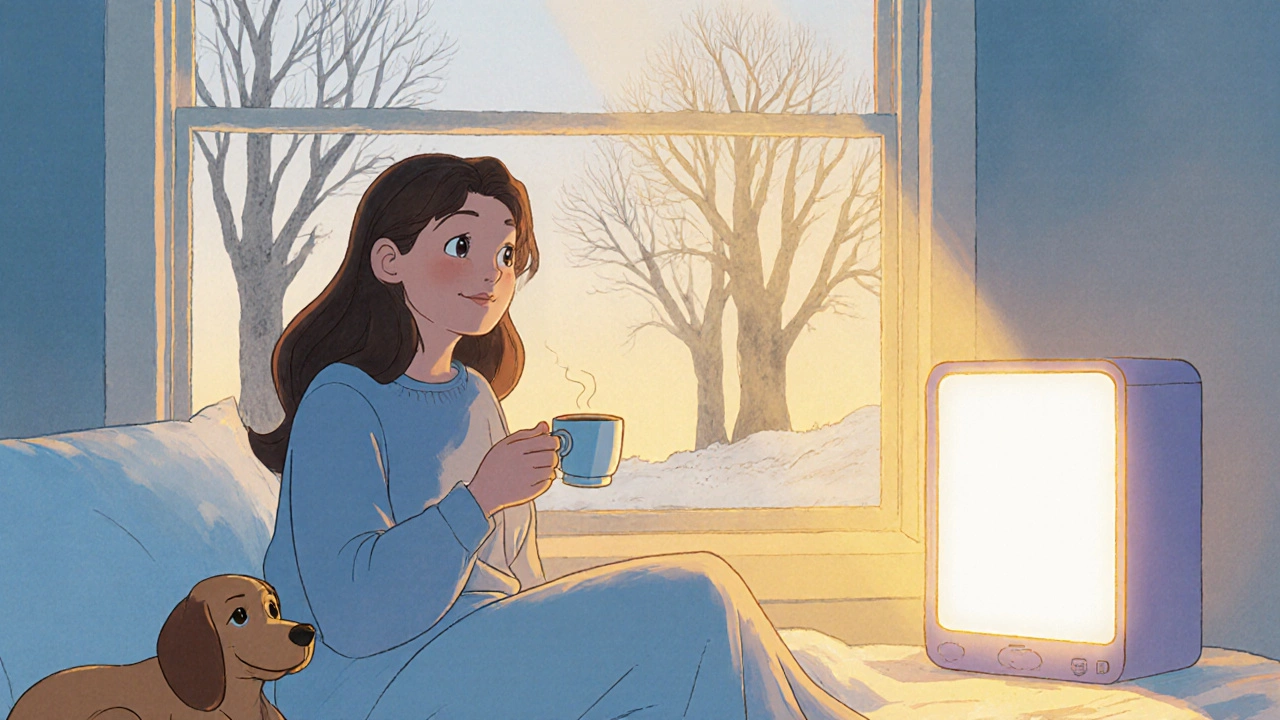
Every year, as the days get shorter and the light fades, millions of people feel a shift-not just in the weather, but in their mood. Fatigue, irritability, cravings for carbs, and that heavy, sinking feeling in the chest aren’t just "being down." For many, it’s seasonal affective disorder, or SAD. And when talk therapy and light boxes don’t cut it, doctors sometimes turn to sertraline. But does it actually help with winter blues? And if so, how?
What Is Seasonal Affective Disorder?
Seasonal affective disorder isn’t just a bad case of the winter blahs. It’s a real subtype of major depressive disorder that follows a seasonal pattern. Symptoms usually start in late fall or early winter and lift in spring or summer. People with SAD often feel exhausted even after sleeping enough, lose interest in things they used to enjoy, gain weight from overeating-especially carbs-and struggle to concentrate. Some even feel hopeless.
Unlike regular depression, SAD has a clear trigger: reduced sunlight. In places like Durban, where winters are mild but daylight still shrinks from 14 hours to under 10, the drop in natural light messes with your body’s internal clock. That affects serotonin, a brain chemical tied to mood, and melatonin, which regulates sleep. When those two get out of sync, depression can follow.
How Sertraline Works in the Brain
Sertraline is an SSRI-selective serotonin reuptake inhibitor. That means it stops your brain from reabsorbing serotonin too quickly, leaving more of it available to help nerve cells communicate. More serotonin often means better mood, less anxiety, and improved sleep.
It’s not a magic pill. It doesn’t make you happy instantly. It takes 4 to 6 weeks to start working. But for people with SAD who’ve tried light therapy and lifestyle changes without success, sertraline can be the missing piece. A 2023 study in the Journal of Affective Disorders followed 212 adults with winter-pattern SAD. Half took sertraline daily from October to March. The other half took a placebo. By February, 64% of the sertraline group reported significant improvement in mood, compared to just 38% in the placebo group.
What’s more, sertraline helped with the physical symptoms too-less fatigue, fewer cravings, better sleep quality. It didn’t just lift sadness; it restored energy.
Why Sertraline Over Other Antidepressants?
There are other SSRIs like fluoxetine (Prozac) and escitalopram (Lexapro) that also treat depression. So why pick sertraline for SAD?
First, it’s well-studied for this specific use. The FDA approved sertraline for SAD in 2006 based on strong clinical trial data. Other SSRIs have less direct evidence for seasonal depression.
Second, it tends to have fewer side effects than older antidepressants. Unlike tricyclics or MAOIs, sertraline doesn’t cause major weight gain, dry mouth, or dizziness in most people. It’s also less likely to interfere with sleep-important when you’re already fighting winter fatigue.
Third, it’s flexible. You can start it before symptoms hit. Many doctors recommend beginning sertraline in early fall, around September, to prevent SAD from taking hold. Others start it once symptoms appear. Either way, it’s easier to adjust than some alternatives.
Who Should Consider Sertraline for SAD?
Not everyone with winter blues needs medication. If your symptoms are mild-maybe you feel a little sluggish or eat more chocolate-light therapy, daily walks, and vitamin D might be enough.
But if you’ve tried those and still feel stuck, sertraline could be worth discussing. You might be a good candidate if:
- Your mood drops every year at the same time
- It interferes with work, relationships, or daily tasks
- You’ve had SAD for multiple winters in a row
- Light therapy didn’t help, or you can’t use it consistently
- You also struggle with anxiety or panic attacks during winter
People with bipolar disorder should be careful. Antidepressants can trigger manic episodes in those with bipolar SAD. Always tell your doctor if you’ve ever had periods of unusually high energy, racing thoughts, or risky behavior.

What to Expect When Starting Sertraline
Most people start with 50 mg a day. Your doctor might increase it to 100 mg after a few weeks if needed. The maximum is usually 200 mg, but few people with SAD need that much.
Side effects are usually mild and temporary. In the first week or two, you might feel:
- Nausea
- Headache
- Insomnia or drowsiness
- Increased anxiety
- Sweating or dry mouth
These tend to fade. If nausea is bad, take it with food. If it keeps you awake, take it in the morning. If you feel drowsy, try taking it at night.
It’s important to keep taking it-even if you feel better after a month. Stopping too soon can bring symptoms back. Most people stay on sertraline for at least one full winter season. Some continue for multiple years if SAD keeps returning.
Combining Sertraline With Other Treatments
Sertraline doesn’t have to be your only tool. In fact, combining it with other strategies often works best.
Use a light therapy box for 30 minutes each morning. Even if you’re on medication, bright light helps reset your circadian rhythm. Sit near a window during lunch. Get outside when the sun’s out-even on cloudy days, natural light is stronger than indoor lighting.
Exercise matters too. A 2022 study found that people with SAD who walked 30 minutes a day, five days a week, improved their mood just as much as those on antidepressants alone. Combine both, and the results are even stronger.
Don’t forget vitamin D. Low levels are common in winter, especially in places with less sun. Many doctors check your vitamin D level before prescribing sertraline. If it’s low, they’ll recommend a supplement-usually 1,000 to 2,000 IU daily.
When Sertraline Doesn’t Work
Not everyone responds to sertraline. About 1 in 3 people with SAD don’t see much improvement after 6 to 8 weeks. That doesn’t mean you’re broken. It just means your brain needs a different approach.
If sertraline isn’t helping:
- Ask about switching to another SSRI, like fluoxetine or escitalopram
- Try bupropion (Wellbutrin), which is the only antidepressant FDA-approved for preventing SAD
- Consider cognitive behavioral therapy tailored for SAD (CBT-SAD), which teaches you to challenge negative winter thoughts
- Explore chronotherapy-adjusting sleep and wake times to match natural light cycles
Some people benefit from a combination of CBT-SAD and medication. A 2021 trial showed that people who got both treatments had lower relapse rates the next winter than those who took medication alone.

Real Stories, Real Results
Anna, 39, from Cape Town, started feeling sluggish every April. By July, she was sleeping 10 hours a night and skipping work. She tried a light box but hated sitting in front of it every morning. Her doctor prescribed sertraline. After six weeks, she started waking up without dread. Her cravings for bread and sweets disappeared. She began walking her dog again. "It didn’t make me euphoric," she says. "But it gave me back the ability to care."
Mark, 52, in Johannesburg, took sertraline for three winters. He felt better but still needed his light box. He stopped the medication one spring, thinking he was cured. The next fall, his mood crashed harder than before. He went back on sertraline-and this time, he didn’t stop until spring came again.
These stories aren’t rare. Sertraline doesn’t cure SAD. But for many, it makes the difference between surviving winter and living through it.
Final Thoughts: Is Sertraline Worth It?
If your winter blues are more than just a mood dip-if they’re stealing your energy, your focus, your joy-then yes, sertraline is worth considering. It’s not the first step. But when other tools fall short, it’s one of the most reliable options we have.
Start with a doctor. Don’t self-prescribe. Don’t compare your dose to someone else’s. Your brain chemistry is unique. What works for one person might not work for you.
And remember: you’re not weak for needing help. Winter isn’t just about colder temperatures. It’s about darkness. And sometimes, the body needs a little chemical support to find its way back to light.
Can sertraline cause weight gain with seasonal affective disorder?
Sertraline is less likely to cause weight gain than some other antidepressants like paroxetine or mirtazapine. In clinical trials for SAD, most people on sertraline didn’t gain weight-and some even lost a few pounds because their cravings for carbs decreased. But if you notice changes in appetite or weight, talk to your doctor. It could mean the dose needs adjusting or that you need to pair it with better nutrition and movement.
How long should I take sertraline for SAD?
Most people take sertraline for the entire winter season-usually from October or November through March or April. Some doctors recommend continuing for a full year if SAD has happened for three or more winters in a row. Stopping too early increases the chance of symptoms returning. Never quit cold turkey. Taper off slowly under medical supervision to avoid withdrawal effects like dizziness or brain zaps.
Is sertraline safe to use with light therapy?
Yes, sertraline and light therapy work well together. In fact, combining them often leads to better results than either one alone. Light therapy helps reset your body clock, while sertraline boosts serotonin. There are no dangerous interactions. Many patients use a 10,000-lux light box for 30 minutes each morning while taking sertraline. Just avoid looking directly at the light-sit nearby while having breakfast or reading.
Can I take sertraline if I have high blood pressure?
Sertraline doesn’t typically raise blood pressure. In fact, it’s often preferred over other antidepressants for people with heart conditions because it’s less likely to affect heart rhythm. But if you’re on blood pressure medication, your doctor should monitor you closely. Some interactions are possible with certain beta-blockers or diuretics. Always list all your medications before starting sertraline.
Does sertraline help with SAD-related sleep problems?
Yes, but it depends on the type of sleep issue. Many people with SAD oversleep and still feel tired. Sertraline can help regulate sleep cycles over time, reducing excessive sleepiness. For those who struggle with insomnia, sertraline can be energizing-so taking it in the morning helps. If sleep problems persist, your doctor might suggest adding a low-dose sleep aid or adjusting timing. Don’t rely on sleeping pills long-term.
Next Steps If You Think Sertraline Might Help
Don’t wait for winter to hit hard. If you notice a pattern-every year, around the same time, your mood drops-start planning now.
- Track your symptoms for one month. Note energy levels, sleep, appetite, and mood.
- Book a visit with your doctor or a psychiatrist. Bring your symptom log.
- Ask about checking your vitamin D and thyroid levels-they can mimic SAD symptoms.
- Ask if light therapy is an option. Even if you’re not sure about medication, it’s a safe first step.
- If sertraline is recommended, ask for a 4-week follow-up. That’s when side effects usually settle and you’ll start to feel changes.
SAD is real. It’s not weakness. And it’s not something you have to endure. With the right tools-including sertraline when needed-you can reclaim your winter.

Christine Mae Raquid
November 1, 2025 AT 12:44Sue Ausderau
November 2, 2025 AT 22:31Tina Standar Ylläsjärvi
November 3, 2025 AT 18:37M. Kyle Moseby
November 5, 2025 AT 08:30Zach Harrison
November 7, 2025 AT 01:26Terri-Anne Whitehouse
November 7, 2025 AT 20:23Matthew Williams
November 8, 2025 AT 22:33Dave Collins
November 9, 2025 AT 15:40Idolla Leboeuf
November 10, 2025 AT 19:44Cole Brown
November 12, 2025 AT 06:19Danny Pohflepp
November 12, 2025 AT 11:37Halona Patrick Shaw
November 14, 2025 AT 03:10Elizabeth Nikole
November 14, 2025 AT 19:52