For years, people with chronic insomnia were told to just sleep hygiene: no caffeine after noon, keep your room dark, avoid screens before bed. Easy enough, right? But if you’ve been lying awake for months-or years-while your partner snores peacefully beside you, you know that’s not enough. Sleep hygiene isn’t a cure. It’s a bandage. And when your insomnia has lasted longer than three months, it’s not a broken habit. It’s a learned pattern. And patterns can be unlearned.
What Chronic Insomnia Really Means
Chronic insomnia isn’t just having a bad night. It’s struggling to fall asleep, stay asleep, or wake up feeling rested at least three nights a week for three months or more. The American Academy of Sleep Medicine defines it this way because it’s not random. It’s persistent. And it’s not just about sleep-it’s about what happens during the day: fatigue, irritability, trouble focusing, even anxiety about sleep itself. This isn’t stress. This isn’t jet lag. This is your brain and body stuck in a loop: you go to bed tired, but your mind races. You check the clock. You worry you’ll be useless tomorrow. You get more anxious. You toss and turn. You finally drift off at 3 a.m.-then wake up at 6, exhausted, and the cycle starts again. And the more you try to force sleep, the more it slips away.Why Sleep Hygiene Alone Fails
Sleep hygiene sounds simple. Keep your room cool-around 65°F. No alcohol after dinner. No screens. Use blackout curtains. White noise machine. All good advice. But here’s the truth: studies show sleep hygiene alone helps maybe 20% of people with chronic insomnia. That’s not because the advice is wrong. It’s because it doesn’t fix the root problem. Your brain has learned to associate your bed with worry, not sleep. You’ve spent months lying there, frustrated, watching the clock. Your body has learned that bed = stress. No amount of dark curtains will fix that. The Sleep Foundation and the American Academy of Sleep Medicine both say sleep hygiene has only moderate evidence for effectiveness. The American College of Physicians, the National Institutes of Health, and the World Health Organization all agree: if you have chronic insomnia, sleep hygiene should be a side note-not the main treatment. Dr. Jack D. Edinger, one of the leading researchers in this field, puts it bluntly: "Sleep hygiene education alone is minimally effective for chronic insomnia and should not be offered as standalone treatment." That’s not a suggestion. It’s a clinical fact.Cognitive Behavioral Therapy for Insomnia (CBT-I): The Only Proven Fix
There’s one treatment that works better than pills, better than supplements, better than meditation apps. It’s called Cognitive Behavioral Therapy for Insomnia, or CBT-I. And it’s not just "talk therapy." It’s a structured, science-backed program with five core parts, delivered over 6 to 8 weeks. And it works. Multiple randomized trials show 70 to 80% of people who complete CBT-I see major improvements in sleep. Not just falling asleep faster-but staying asleep, waking up less, and feeling more rested during the day. The best part? The results last. A 2020 meta-analysis found that CBT-I reduced the time it took to fall asleep by 18.2 minutes and cut nighttime wake-ups by 27.4 minutes. Medications? They helped by only 12.1 and 15.8 minutes-and the benefits vanished once people stopped taking them. CBT-I doesn’t just treat symptoms. It rewires your relationship with sleep.The Five Pillars of CBT-I
- Stimulus Control: Your bed is for sleep and sex only. No reading. No scrolling. No lying there worrying. If you’re not asleep in 15 to 20 minutes, get up. Go to another room. Do something quiet-read a book under dim light-until you feel sleepy. Then go back to bed. Repeat. This retrains your brain: bed = sleep.
- Sleep Restriction: You’re spending 8 hours in bed but only sleeping 5. CBT-I says: limit your time in bed to 5 hours. Yes, you’ll be tired. Yes, it’s brutal for the first two weeks. But by increasing your sleep drive, your body starts consolidating sleep. As your efficiency improves, you slowly add back 15 minutes of bed time each week. This isn’t punishment-it’s physics.
- Cognitive Restructuring: "I need 8 hours or I’ll fail at work." "If I don’t sleep tonight, I’m ruined." These thoughts keep you awake. CBT-I helps you challenge them. You learn to replace catastrophic thinking with facts: "I’ve survived 3 hours of sleep before. My body adapts. I don’t need perfect sleep to function." Studies show this cuts sleep-related anxiety in 65% of patients.
- Relaxation Training: Your body is tense. Your heart is racing. You’re not physically ready for sleep. Techniques like diaphragmatic breathing, progressive muscle relaxation, or mindfulness help calm your nervous system. Not to force sleep-but to remove the barrier to it.
- Sleep Hygiene: Yes, it’s still part of the program. But now it’s just one tool among many. You’re not doing it alone. You’re doing it with structure, support, and science.

Real People, Real Results
One Reddit user wrote: "After 8 weeks of CBT-I, my sleep efficiency went from 68% to 89%. I used to take two hours to fall asleep. Now it’s 15 minutes." Another said: "The sleep restriction was hell. I was a zombie. But after month two? I slept like a baby. I haven’t woken up before 6 a.m. in six months. I got my life back." But it’s not easy. About 62% of people say the first two weeks are the hardest. You’re tired. You’re frustrated. You want to quit. That’s normal. The key is sticking with it. Dr. Colleen Carney’s research shows most people start seeing changes in 2 to 4 weeks. Full results? 8 to 12 weeks.What About Medications?
Pills like zolpidem, eszopiclone, or suvorexant can help in the short term. Maybe for a week or two after a major stressor. But they don’t fix the pattern. And they come with risks: dependence, memory issues, next-day grogginess, even falls in older adults. The American Academy of Sleep Medicine says: "Pharmacotherapy should be used only as a short-term adjunct, not a long-term solution." A 2021 JAMA Internal Medicine study compared internet-based CBT-I to placebo. The CBT-I group had a 55% remission rate. The placebo group? 18%. That’s not a small difference. That’s life-changing.Access Is the Real Problem
Here’s the catch: there aren’t enough trained CBT-I therapists. In the U.S., there are only 0.5 certified CBT-I providers per 100,000 people. In rural areas, 78% of counties have zero sleep specialists. Insurance often covers only 3 sessions out of the recommended 6 to 8. That’s why digital CBT-I programs like Sleepio and SHUTi are exploding. They’ve been cleared by the FDA. Studies show they work just as well as in-person therapy. Apps like Somryst have shown 55% remission rates. Fitbit now integrates sleep restriction principles into its Sleep Profile feature. Companies like Pear Therapeutics are testing AI-driven CBT-I that personalizes sessions based on your sleep data. And 37% of Fortune 500 companies now offer CBT-I through employee health programs.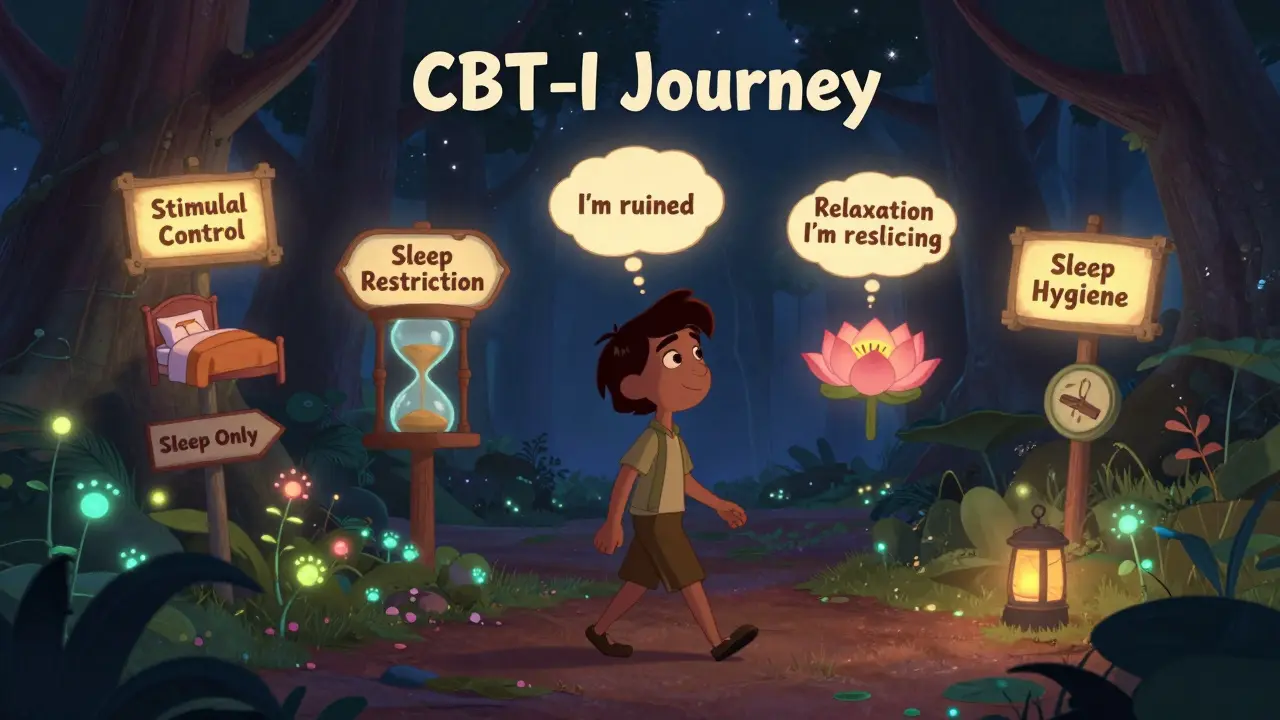
How to Get Started
1. Track your sleep for two weeks. Use a notebook or app. Note when you get in bed, when you fall asleep, when you wake up, how many times you wake, how you feel in the morning. 2. Find a CBT-I provider. Search the Society of Behavioral Sleep Medicine directory. Ask your doctor for a referral. Look for licensed psychologists or sleep specialists with CBT-I training. 3. If you can’t find one, try a digital program. Sleepio, SHUTi, and Somryst are evidence-based and FDA-cleared. Many are covered by insurance now. 4. Start with sleep hygiene-but don’t stop there. Keep your room cool. No caffeine after 2 p.m. No alcohol within 4 hours of bed. But pair this with stimulus control and sleep restriction. That’s where the real change happens. 5. Be patient. The first week is the hardest. You’ll feel worse before you feel better. That’s part of the process. Don’t give up.The Future of Sleep
In 10 years, experts predict CBT-I will be the standard treatment for 90% of chronic insomnia cases. Pills will be reserved for emergencies. Insurance will cover full courses. Doctors will refer you to CBT-I before prescribing anything. Right now, you’re stuck in an outdated system. But you don’t have to be. You don’t need more pills. You don’t need magic teas. You need a new way of thinking about sleep. And that’s exactly what CBT-I gives you.Frequently Asked Questions
Is CBT-I just for people who are stressed?
No. CBT-I works for anyone with chronic insomnia, regardless of cause. It doesn’t matter if your insomnia started after a breakup, a job loss, menopause, or just out of nowhere. The problem isn’t the trigger-it’s the learned pattern. CBT-I rewires your brain’s sleep response, no matter how it started.
Can I do CBT-I on my own without a therapist?
Yes, but with caveats. Digital programs like Sleepio, SHUTi, and Somryst are clinically proven and FDA-cleared. They follow the same protocol as in-person therapy. Many people succeed with them. But if you have depression, PTSD, or severe anxiety, working with a therapist is strongly recommended. Self-guided programs work best for people who are motivated and can follow a structured plan.
How long until I see results from CBT-I?
Most people notice small improvements in 2 to 4 weeks. Sleep efficiency often climbs during the sleep restriction phase, even if total sleep time hasn’t changed yet. Full benefits-like falling asleep faster, waking less, and feeling rested-usually appear after 8 to 12 weeks. The first two weeks are the toughest, but that’s when your brain is learning a new habit.
Is CBT-I covered by insurance?
Some plans cover it, especially if delivered by a licensed psychologist or through an FDA-cleared digital program. Medicare and Medicaid coverage is expanding. Check with your provider. Many employers now include CBT-I in employee wellness programs. If you’re denied, ask for a letter of medical necessity from your doctor-it often helps.
What if I can’t stick to the schedule? What if I work nights?
CBT-I can be adapted. If you work nights, your "bedtime" is when you plan to sleep during the day. The principles stay the same: consistent wake time, only sleep in bed, limit time in bed to match actual sleep. The biggest challenge is maintaining a regular wake time-even on days off. That’s critical. Your body thrives on rhythm, no matter your schedule.
Can I use melatonin or CBD with CBT-I?
It’s okay to use them temporarily while starting CBT-I, but they shouldn’t replace it. Melatonin helps regulate timing, not depth of sleep. CBD may reduce anxiety but doesn’t fix the learned sleep pattern. The goal of CBT-I is to stop needing supplements. Think of them as training wheels-not the bike.


William Liu
December 18, 2025 AT 13:56After 5 years of insomnia, I tried CBT-I last year. The sleep restriction part nearly broke me. I was a zombie for two weeks. But then something clicked. I started sleeping 7 hours straight for the first time in years. No pills. No magic. Just science. If you're still suffering, don't give up. It's worth the hell.
Aadil Munshi
December 19, 2025 AT 20:50Oh great, another post pretending CBT-I is some revolutionary breakthrough. Let me guess-you also think yoga fixes depression and kale cures cancer. The truth? Sleep is a biological function, not a cognitive puzzle to be hacked. Your brain doesn't 'learn' insomnia like it learned to ride a bike. It's a symptom. Maybe of circadian disruption, maybe of low melatonin, maybe of undiagnosed sleep apnea. But no, let's just retrain your thoughts while ignoring the actual physiology. Classic Western medicine overcomplicating the obvious.
Frank Drewery
December 20, 2025 AT 04:26I read this when I was at my lowest. I’d been lying awake for 18 months. I didn’t believe in any of it. But I tried the 15-minute rule-got up, read in the kitchen, came back. First night, I fell asleep in 40 minutes. Not 2 hours. Just 40. That tiny win kept me going. I didn’t fix everything overnight. But I started trusting my body again. That’s more than any pill ever gave me.
Danielle Stewart
December 21, 2025 AT 10:04For anyone reading this and thinking, 'I can't do this'-you already are. Just being here, reading this, means you're ready to change. CBT-I isn't about perfection. It's about consistency. Miss a day? Fine. Get back on track tomorrow. The goal isn't to sleep perfectly-it's to stop fighting sleep. You're not broken. You're just stuck in a loop. And loops can be broken. I believe in you.
mary lizardo
December 22, 2025 AT 05:12While the article presents a compelling narrative, it suffers from significant methodological oversimplification. The assertion that CBT-I is 'the only proven fix' ignores the substantial body of literature supporting pharmacological interventions in specific subpopulations-particularly those with comorbid psychiatric conditions. Furthermore, the claim that sleep hygiene has 'only moderate evidence' is misleading; meta-analyses by Morin et al. (2006) and the Cochrane Review (2015) indicate moderate-to-strong efficacy when properly implemented. The conflation of 'standalone treatment' with 'adjunctive component' reflects a fundamental misunderstanding of clinical protocols. The author’s rhetorical framing borders on pseudoscientific evangelism.
jessica .
December 23, 2025 AT 00:52CBT-I? That's just the government's way of getting you to stop taking real medicine. They don't want you to know that Big Pharma is hiding the real cure-melatonin + magnesium + grounding mats. The FDA cleared those apps because they're funded by the same people who control the CDC. They don't want you sleeping well. They want you docile. Wake up. Your insomnia isn't psychological-it's chemical poisoning from 5G towers and fluoridated water. CBT-I is a distraction. Real sleep comes from nature, not apps.
Ryan van Leent
December 24, 2025 AT 00:28Why are we still talking about this like it's new? I've been doing sleep restriction since 2017. It works. But nobody tells you how brutal it is. You're exhausted. You snap at your kid. You cry in the shower. You think you're losing your mind. And then one day you wake up and you're not tired anymore. No one warned me about the emotional toll. Just the sleep stats. That's not helpful. It's like saying 'just lose weight' and ignoring the trauma behind overeating. This stuff is hard. It's not just a hack.
Sajith Shams
December 24, 2025 AT 16:42CBT-I is just a fancy name for discipline. If you can't control your mind enough to stop checking the clock, you shouldn't be allowed to have a bed. Everyone in India sleeps 5 hours and wakes up at 4am without apps or therapists. We don't have time for your Western neuroses. Stop overthinking sleep. Go to bed when tired. Wake up when light. That's it. No therapy needed. Your brain is weak, not broken.