When you pick up a prescription, you might see two options: the familiar brand-name drug with its colorful packaging, or a plain white pill with a simple label. The brand version costs $150. The generic? $25. You might wonder - is the cheaper one just as good? Or are you saving money at the cost of your health?
They’re the Same Medicine - Just Cheaper
Generic drugs aren’t knockoffs. They’re not cheaper because they’re lower quality. They’re cheaper because they don’t have to pay for research, marketing, or patent protection. By law, the FDA requires generic drugs to contain the exact same active ingredient, in the same strength, and work the same way in your body as the brand-name version. That means if you take 10 mg of lisinopril from the brand or the generic, your blood pressure will respond identically.
The FDA doesn’t just trust the manufacturer’s word. Every generic drug must pass a bioequivalence test. That means scientists measure how fast and how much of the drug enters your bloodstream. The generic’s performance must fall within 80-125% of the brand’s. In plain terms: if the brand gets 100 units into your blood, the generic must get between 80 and 125. That’s not a wide gap - it’s tighter than most over-the-counter pain relievers vary between batches.
And it’s not just about the pill. Generics must match the brand in dosage form (tablet, capsule, liquid), route of administration (oral, injectable), and stability. They’re held to the same manufacturing standards. The same factories sometimes make both versions - just under different labels.
Why the Price Difference Is So Huge
Brand-name drugs cost a lot because the company had to pay for years of research, clinical trials, and regulatory approval. That can run over $2 billion per drug. Once the patent expires - usually after 10 to 12 years - other companies can step in and make the same drug without repeating those expensive steps.
Instead of doing full clinical trials, generic makers file an Abbreviated New Drug Application (ANDA). They prove bioequivalence and show their manufacturing process meets FDA standards. That cuts development costs by 90% or more. Those savings get passed on.
Here’s the real kicker: competition drives prices down fast. When the first generic hits the market, prices drop to about 90% of the brand’s cost. With two or three competitors, it falls to 60-70%. Once five or more companies are making it, prices often drop below 50% - sometimes even 20% - of the original brand price.
Take Nexavar, a cancer drug. When the first generic entered in 2022, Bayer - the brand maker - cut its list price by 50% the next year. Why? Because they knew they couldn’t keep charging $10,000 a month when a generic version was selling for $2,000. The same thing happened with Januvia. Merck lowered its price by over 40% as generics arrived.
What You’re Actually Paying - List Price vs Net Price
Here’s where things get confusing. You see a $150 price tag on the brand drug at the pharmacy. But that’s not what the insurer or Medicare pays. That’s the list price. The real price - the net price - is what’s left after rebates, discounts, and pharmacy benefit manager (PBM) negotiations.
Drug manufacturers offer huge rebates to insurers and PBMs to get their drugs on preferred formularies. In 2024, brand-name drug list prices went up by 2.3%, but net prices barely moved - up just 0.1%. That means manufacturers are giving away more money just to stay on the list.
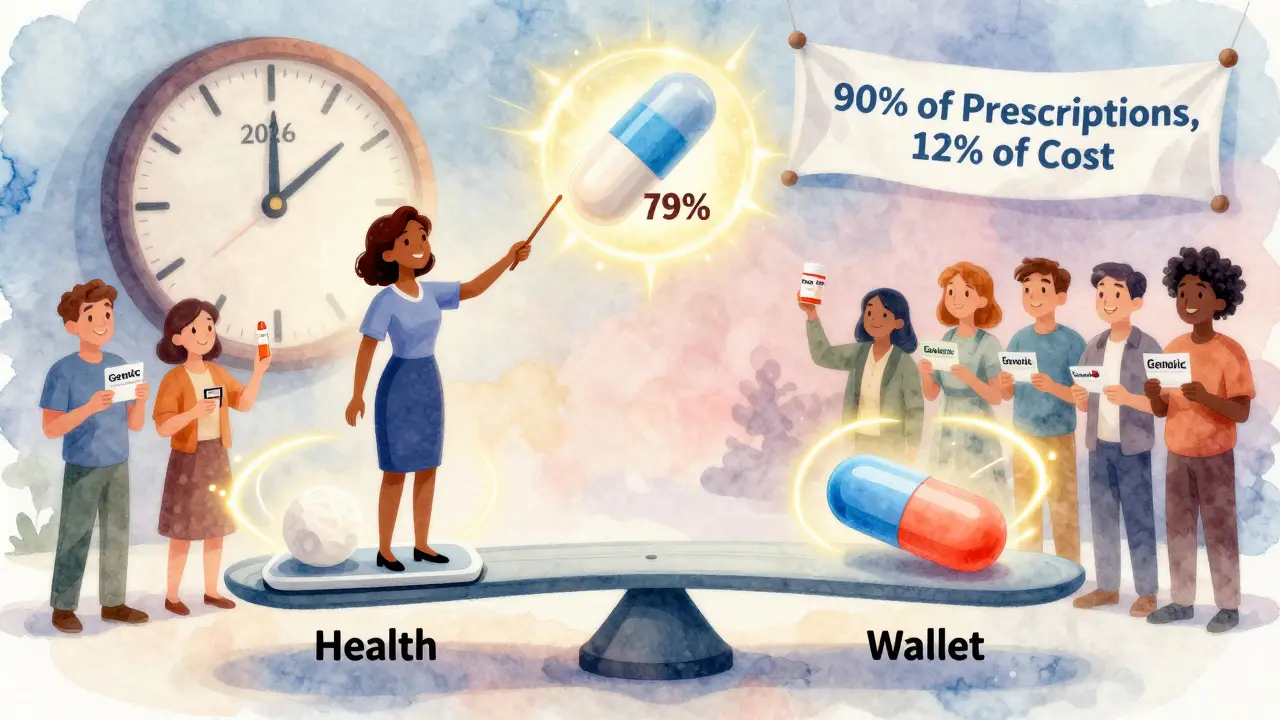
Generics don’t play that game. They have no rebates. No complex negotiations. They’re sold at a flat, low price. That’s why, even though generics make up 90% of all prescriptions filled in the U.S., they only account for 12% of total drug spending. In 2024, Americans spent $98 billion on 3.9 billion generic prescriptions. For brand drugs - just 435 million prescriptions - we spent $700 billion.
That’s not a typo. You’re paying less than 10 cents on the dollar for 9 out of 10 pills you take.

Why People Still Trust the Brand - Even When It Costs More
Despite the data, many people still believe the brand is better. A January 2025 survey of over 1,000 Americans found that 84% agree generics are just as effective. But 62% still trust the brand more. Why?
It’s psychology. The brand name feels familiar. The packaging looks professional. You’ve seen the commercials. The generic looks like a hospital pill - plain, unmarked, sometimes even a different color or shape.
And then there’s the fear: “What if it doesn’t work for me?”
That’s understandable. But the science doesn’t support it. The FDA, the American Medical Association, and every major medical society in the U.S. agree: generics are therapeutically equivalent. If your doctor prescribed the brand, switching to the generic isn’t a compromise - it’s a smart financial move.
Still, 63% of people choose generics - not because they believe they’re better, but because they can’t afford the brand. Sixty percent say they’d prefer the brand if cost weren’t an issue. That tells you something: the system works, but it’s built on financial pressure, not trust.
When Generics Might Not Be the Best Choice
There are rare exceptions. For drugs with a very narrow therapeutic window - where even tiny differences in blood levels can cause harm - doctors sometimes stick with the brand. Think of drugs like warfarin (blood thinner), levothyroxine (thyroid), or some anti-seizure medications.
Even then, the FDA says generics are safe. But some doctors, out of habit or caution, prefer to keep patients on the same version. If you’re on one of these drugs and your doctor insists on the brand, ask why. Is it because of evidence - or just tradition?
Also, some brand-name drugs don’t have generics yet. That’s usually because the patent is still active. But if you’re paying full price for a drug that’s been on the market for over a decade, it’s worth checking if a generic is coming soon.
How to Save Even More
Even with generics, costs can add up. Here’s how to cut them further:
- Ask your pharmacist if there’s a 30-day supply vs a 90-day supply. Sometimes buying in bulk saves money - but not always. Compare prices.
- Use mail-order pharmacies. Many insurers offer discounts for 90-day fills shipped to your home.
- Check GoodRx or SingleCare. These apps show real-time prices at nearby pharmacies. Sometimes the same generic costs $5 at Walmart and $22 at CVS.
- Ask your doctor about patient assistance programs. Many drugmakers offer free or low-cost versions of their brand drugs to qualifying patients - even if a generic exists.
- If you’re on Medicare Part D, your out-of-pocket costs will be capped at $2,000 in 2026. That means once you hit that limit, your generics will cost you nothing for the rest of the year.
What’s Changing in 2025-2026
The Inflation Reduction Act is changing the game. Starting in January 2026, Medicare will negotiate prices for 10 high-cost brand drugs. That means those drugs - like Eliquis, Jardiance, and others - will see steep price drops. Some could fall by 79% or more.
Manufacturers are already reacting. Merck lowered Januvia’s price in 2025, likely to avoid the worst of the Medicare cut. Other companies are doing the same.
Meanwhile, more patents are expiring. In 2025 alone, over 20 major brand drugs will lose exclusivity. That means dozens more generics will hit the market, driving prices even lower.
And here’s the irony: while brand-name drug list prices are still high, the U.S. actually has lower net prescription prices than countries like Canada, Germany, and the UK - thanks almost entirely to how cheap generics are. The U.S. pays more for the brand, but saves massively because 90% of prescriptions are generic.
Bottom Line: Choose Generic - Unless There’s a Real Reason Not To
There’s no medical reason to pay extra for the brand if a generic is available. The science is clear. The savings are massive. The risk is minimal.
Generic drugs are the reason millions of Americans can afford their prescriptions. They’re not a compromise. They’re the smart, safe, and standard choice in modern medicine.
If your doctor prescribes a brand, ask: “Is there a generic?” If they say no, ask why. If they say yes, take it. You’re not saving money by choosing the brand. You’re paying more for a label.
Are generic drugs really as effective as brand-name drugs?
Yes. Generic drugs must contain the same active ingredient, in the same strength and dosage form, and work the same way in your body as the brand-name version. The FDA requires them to pass strict bioequivalence tests, proving they deliver the same amount of medicine into your bloodstream at the same rate. Millions of people use generics every day with the same results as the brand.
Why are generic drugs so much cheaper?
Generic drugs don’t have to repeat expensive clinical trials or pay for marketing campaigns. Once a brand-name drug’s patent expires, other companies can produce the same medicine using a faster, cheaper approval process called an ANDA. That cuts development costs by 90% or more, and competition among generic makers drives prices down - often to 80-85% less than the brand.
Can I switch from a brand-name drug to a generic safely?
In most cases, yes. The FDA considers generics therapeutically equivalent. If you’re on a standard medication like metformin, atorvastatin, or lisinopril, switching is safe and common. For drugs with a narrow therapeutic window - like warfarin or levothyroxine - some doctors prefer to keep you on the same version. But even then, generics are approved and safe. Always talk to your doctor before switching.
Why do some people say generics don’t work as well?
It’s usually not about the drug - it’s about perception. Generics look different: different color, shape, or markings. Some people confuse that with lower quality. Others feel more confident with a brand they’ve seen advertised. But studies show no difference in effectiveness. When patients are told they’re taking a generic, they report fewer side effects - simply because they expect them to be weaker. That’s a psychological effect, not a medical one.
Do insurance companies prefer generics?
Absolutely. Insurance plans and Medicare Part D put generics on their preferred lists because they’re cheaper. That means lower copays for you - sometimes as low as $0 or $5. Many plans won’t cover the brand unless you’ve tried the generic first and it didn’t work. That’s called step therapy, and it’s standard practice.
Is it true that brand-name drug prices are falling?
Yes - but only for brands facing generic competition. Manufacturers like Bayer and Merck have cut prices on drugs like Nexavar and Januvia by 40-50% in recent years, partly to stay competitive and partly to prepare for Medicare price negotiations starting in 2026. However, brand drugs with little or no competition - especially rare disease medications - can still have massive price hikes. The trend is mixed, but generics are the reason overall drug spending is going down.