Something’s off with your nails. They’re thick, discolored, maybe crumbling or lifting from the bed. You Google it. Fungal infection? Psoriasis? Both sound bad. And both look eerily similar. You’re not alone. In fact, fungal nail infection and nail psoriasis get mixed up more than you’d think - even by doctors. The truth? They’re completely different conditions with different causes, treatments, and outcomes. Getting this right matters because the wrong treatment can make things worse.
What’s Really Going On With Your Nails?
If your nails are yellow, thick, or lifting, it’s easy to assume it’s fungus. After all, that’s what most people hear about. But here’s the catch: up to 68% of nail psoriasis cases show the same yellowish discoloration. The difference isn’t always obvious to the eye. That’s why so many people waste months - sometimes years - on antifungal creams and pills that do nothing. Nail psoriasis isn’t just a nail problem. It’s part of a bigger autoimmune condition. When your immune system attacks your skin cells, they multiply too fast - every 3 to 4 days instead of the normal 28 to 30. That messes up the nail matrix, the living tissue under your cuticle that makes your nail grow. The result? Pitting, oil spots, and nail separation. Fungal nail infections, or onychomycosis, are caused by real invaders: fungi like Trichophyton rubrum. These microbes don’t care about your immune system. They just love warm, damp places - your sweaty socks, your shower floor, your gym bag. They eat keratin, the protein your nails are made of. That’s why the nail gets thick, brittle, and sometimes smells bad.The Telltale Signs: Pitting, Odor, and Pattern
Here’s how to start telling them apart - even before you see a doctor. Nail psoriasis often shows:- Nail pitting: Tiny dents, like pinpricks, on the nail surface. Found in 70% of cases.
- Salmоn patches: Translucent red or yellow stains under the nail, like oil on water.
- Oil-drop lesions: Brownish-yellow spots that look like a drop of oil trapped under the nail.
- Multiple nails affected: Usually fingernails first. Often several nails change at once.
- No foul smell: Psoriasis doesn’t cause odor.
- Thickened nails: Can get up to 5mm thick - way more than psoriasis.
- Starting at the edges: Often begins at the side or tip of the nail, creeping inward.
- Dark discoloration: Turns brown or black as the fungus progresses.
- Foul odor: Present in about 40% of cases - a dead giveaway.
- One or two nails first: Usually starts on one toe, then spreads.
Why Misdiagnosis Is So Common (and Costly)
You’d think doctors would know the difference. But here’s the reality: primary care physicians correctly diagnose these conditions only 52% of the time. Dermatologists? Around 85%. That gap is huge. Why? Because both conditions look similar. A yellow, thickened nail could be either. And many patients don’t have visible skin psoriasis yet. So doctors assume fungus - especially if the patient is older, diabetic, or wears closed shoes. The consequences? People take antifungal pills for months - with side effects like liver damage - when they need steroid injections or biologics. Others get steroid creams for what’s actually fungus, making the infection worse. One Reddit user wrote: “I spent 8 months on antifungals. My nails got worse. Then I found out it was psoriasis.” The American Podiatric Medical Association estimates 150,000 cases are misdiagnosed every year in the U.S. alone. That’s $850 million wasted on wrong treatments.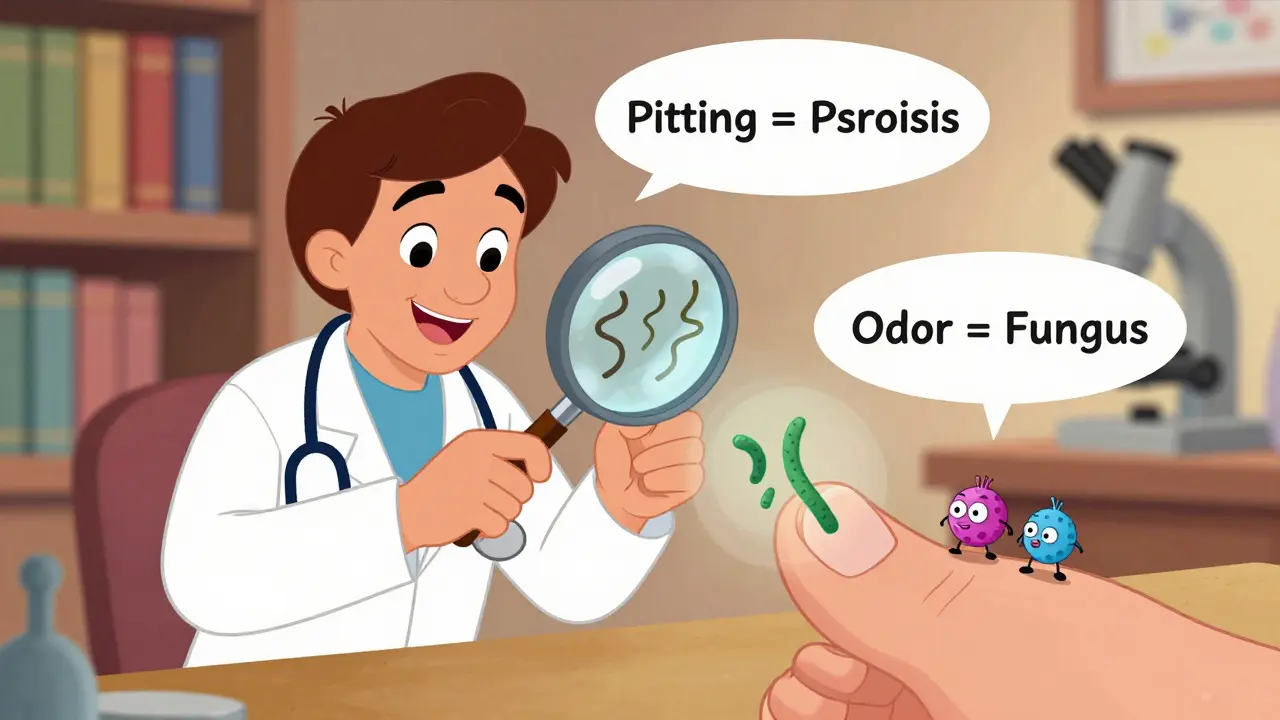
How Doctors Really Diagnose This
If you’re unsure, don’t guess. See a dermatologist. Here’s what they’ll do:- Clinical exam: They’ll look for pitting, oil spots, and how many nails are involved.
- KOH prep: A quick scrape of the nail is mixed with potassium hydroxide and looked at under a microscope. This catches fungus in 70-80% of cases. Fast. Cheap. $15-$25.
- Fungal culture: If KOH is negative but suspicion remains, they’ll send a sample to a lab. Takes 2-6 weeks, but it’s 95% specific.
- PAS staining: A special dye that highlights fungal elements in tissue. 90% sensitive. Used when the diagnosis is still unclear.
Treatment: What Actually Works
Fungal nail infection:- Terbinafine: Oral pill. 78% success rate after 12 weeks. Best for toenails.
- Itraconazole: Another oral option. Works in pulses - one week on, three off.
- Topical antifungals: Jublia (efinaconazole) or Penlac (ciclopirox). Must be applied daily for 9-12 months. Slower, but safer for people who can’t take pills.
- Nail removal: Rarely needed. Only if the infection is severe and unresponsive.
- Corticosteroid injections: Directly into the nail fold. Can show improvement in 8-12 weeks.
- Topical vitamin D analogs: Like calcipotriol. Applied daily under the nail.
- Biologics: Drugs like secukinumab (Cosentyx) or ixekizumab. These target the immune system. 65% of patients see major improvement after 24 weeks.
- Phototherapy: UV light treatment. Helps if skin psoriasis is also active.

Home Care: What to Do (and Not Do)
For fungal infections:- Keep feet dry. Humidity above 40% helps fungus grow.
- Wear breathable shoes. Avoid tight, synthetic materials.
- Change socks daily. Use moisture-wicking fabrics.
- Disinfect shoes with antifungal spray.
- Don’t share nail clippers or towels.
- Avoid trauma. Don’t bite nails, pick at cuticles, or use harsh nail polish removers.
- Use emollients daily. Moisturizing helps prevent nail separation.
- Use a gentle nail file. Don’t aggressively trim or file the nail.
- Track changes. Take monthly photos under consistent lighting. This helps your doctor see progress.
What’s Next? The Future of Nail Diagnosis
New tools are coming fast. Researchers at Mount Sinai are studying the nail microbiome - the bacteria and fungi living under your nail. They found psoriasis nails have more Staphylococcus and less Cutibacterium, while fungal nails show high levels of Trichophyton DNA. AI is also stepping in. The Global Psoriasis Atlas predicts AI-powered nail image analysis will cut misdiagnosis rates by 22% by 2027. Imagine snapping a photo of your nail with your phone - and an algorithm tells you whether it’s fungus or psoriasis. That’s not science fiction anymore. Climate change is making things harder too. Warmer, wetter weather expands fungal habitats. The International Society for Human and Animal Mycology expects fungal nail infections to rise 15% over the next decade.What You Should Do Right Now
If you’re unsure what’s wrong with your nails:- Look for pitting. If you see it, it’s likely psoriasis.
- Check for odor. If it smells bad, it’s likely fungal.
- Don’t start treatment until you know for sure.
- See a dermatologist - not a podiatrist or general practitioner - for the best diagnosis.
- Take a photo of your nails today. Take another in 30 days. Compare.
Can nail psoriasis turn into a fungal infection?
Yes. Nail psoriasis damages the nail structure, making it easier for fungi to invade. About 4.6% to 30% of people with nail psoriasis develop a secondary fungal infection. This is called a superinfection. It often makes the nail worse - more thickened, crumbly, or discolored. If you have psoriasis and your nails suddenly change or smell bad, get tested for fungus.
Do antifungal pills work for nail psoriasis?
No. Antifungal pills like terbinafine or itraconazole target fungi, not autoimmune activity. If you have nail psoriasis and take these pills, they won’t help - and they can harm your liver. Many patients waste months on them before getting the right diagnosis. Always confirm the cause with a KOH test or biopsy before starting treatment.
Why do my nails keep getting worse even after treatment?
Two common reasons: misdiagnosis or incomplete treatment. If you have psoriasis but were treated for fungus, the real problem wasn’t addressed. Or if you stopped antifungals too early - say, after 3 months - the fungus may still be alive under the nail. Fungal infections require 6-12 months of treatment because nails grow slowly. Psoriasis treatments like biologics take 12-24 weeks to show results. Patience and accuracy matter.
Can I treat this at home without seeing a doctor?
You can manage symptoms at home - keeping nails dry, moisturizing, avoiding trauma - but you can’t reliably diagnose the cause without testing. Over-the-counter antifungal creams won’t fix psoriasis. And steroid creams can worsen fungal infections. If your nails haven’t improved in 2-3 months, or if they’re spreading, see a dermatologist. Self-treatment often delays the right care.
Are nail changes a sign of something more serious?
Yes. Nail psoriasis is linked to psoriatic arthritis - a form of joint inflammation that can cause permanent damage if untreated. Fungal infections in people with diabetes or poor circulation can lead to serious foot ulcers or infections. If you have nail changes and also have joint pain, swelling, or numbness in your toes, get checked. Your nails are a window into your overall health.


Chloe Hadland
January 22, 2026 AT 19:32My nails have been weird for years and I just thought it was aging or too much gel polish. Turns out it was psoriasis. This post saved me from another year of antifungals that did nothing. Thank you.
Sawyer Vitela
January 24, 2026 AT 15:23Stop guessing. Get a KOH test. If you don't, you're just wasting time and money. The stats are clear.
Kevin Waters
January 24, 2026 AT 18:36I had this exact issue. Thought it was fungus, took terbinafine for 6 months, nails got worse. Derm said 'you have psoriasis' and gave me a steroid shot. Two months later, my nails looked normal. Don't self-diagnose.
Shanta Blank
January 26, 2026 AT 08:52OH MY GOD. I just realized my 'fungal' nail was actually psoriasis. I've been taking pills like a madwoman while my immune system screamed for help. I'm crying. Not from sadness, from rage. Why does no one tell you this?!?!?!
Also, I now suspect my mom's 'old lady nails' were psoriasis too. She's been on antifungals since 2017. She's 72. She's got joint pain. She's got psoriasis on her elbows. WHY DID NO ONE CONNECT THE DOTS?!?!
I'm going to send this to every relative who's ever had 'nail fungus.' This is a medical scandal.