Blood Thinner & COVID-19 Treatment Calculator
Calculate Your Safe Medication Plan
This tool helps determine safe adjustments for blood thinners when taking COVID-19 antiviral treatments like Paxlovid. Always consult your healthcare provider before making any changes.
Your Recommendations
Enter your details above to see your personalized medication guidance.
Important Safety Note: This calculator provides general guidance based on clinical guidelines. Your healthcare provider will determine your specific treatment plan based on your full medical history and current condition.
When you’re on a blood thinner like apixaban, rivaroxaban, or warfarin, even a common cold can become a high-stakes situation - especially if it turns into a serious respiratory infection like COVID-19. During the pandemic, doctors quickly realized that these infections don’t just attack the lungs; they trigger a dangerous clotting response in the body. That’s why many hospitalized patients were put on stronger doses of anticoagulants. But here’s the problem: the very drugs used to treat COVID-19 - like Paxlovid and dexamethasone - can mess with how those blood thinners work, sometimes turning a life-saving treatment into a life-threatening one.
Why COVID-19 Makes Blood Clots More Likely
COVID-19 isn’t just a lung infection. In severe cases, it turns your blood into a sticky, clot-prone mess. Studies show that up to 70% of critically ill patients develop tiny clots in their lung blood vessels, which can lead to organ failure. This isn’t random. The virus triggers massive inflammation, releasing chemicals that push your body into a hypercoagulable state - meaning your blood clots too easily. That’s why doctors started giving therapeutic doses of anticoagulants to hospitalized patients, not just the low preventive doses. The American Society of Hematology confirmed this approach in 2021: for acute COVID-19 illness, therapeutic anticoagulation saves lives.
But the danger doesn’t end when you leave the hospital. A Johns Hopkins study found that 65% of patients still had elevated D-dimer levels - a marker of clotting - for up to three weeks after discharge. That means the clotting risk lingers, and stopping anticoagulants too soon can be deadly.
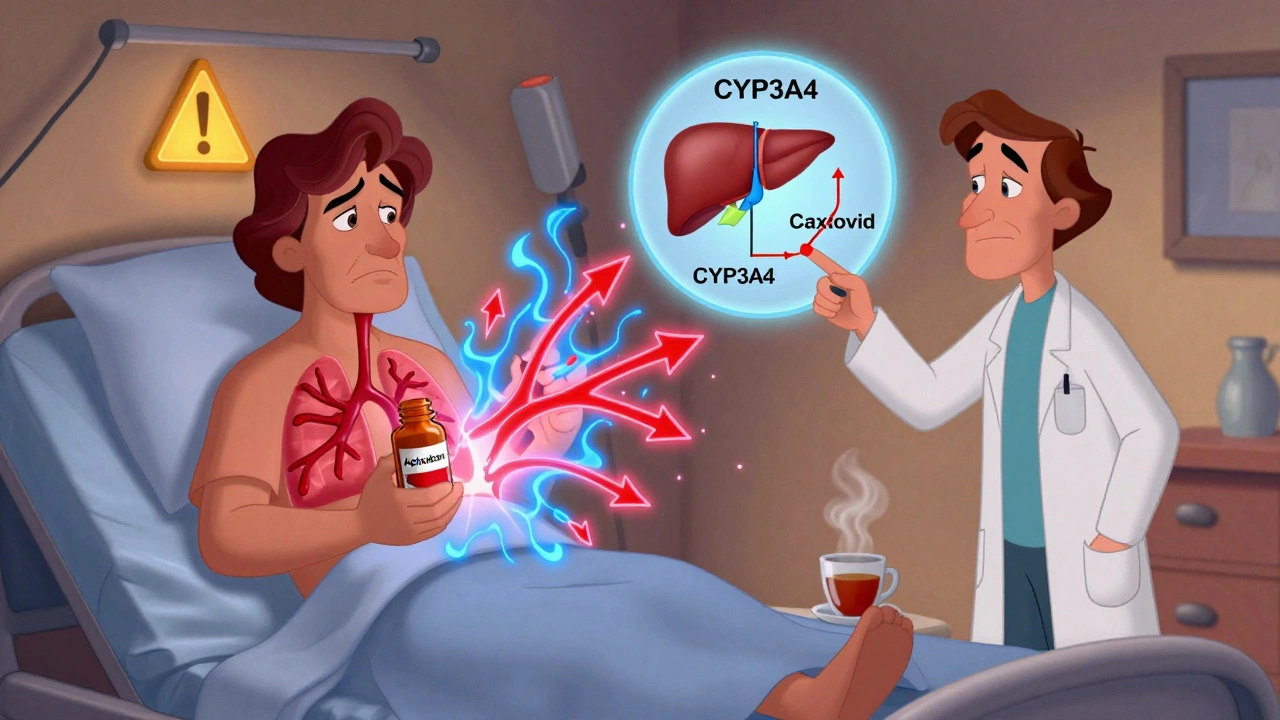
How Paxlovid and Other Antivirals Interfere with Blood Thinners
Paxlovid - the antiviral combo of nirmatrelvir and ritonavir - is one of the most effective treatments for early COVID-19. But ritonavir, its booster component, is a powerful inhibitor of CYP3A4 and P-glycoprotein, two key systems your body uses to break down drugs. Many direct oral anticoagulants (DOACs) - apixaban, rivaroxaban, dabigatran, edoxaban - rely on these same systems to be cleared from your body. When ritonavir blocks them, your blood thinner builds up to dangerous levels.
A 2022 study in PMC9284020 found that all 12 patients on DOACs who took Paxlovid or similar antivirals had their drug levels spike dramatically. One patient on rivaroxaban ended up in the ER with gastrointestinal bleeding after continuing his full dose during Paxlovid treatment. He needed two units of blood. That’s not an outlier. The FDA reported 147 cases of major bleeding linked to Paxlovid and DOACs between January 2022 and June 2023.
On the flip side, dexamethasone - a steroid used for severe COVID-19 - does the opposite. It speeds up how fast your body clears DOACs, potentially cutting their effect by half. That means you could be at risk for a stroke or pulmonary embolism even while on your usual dose.
Warfarin vs. DOACs: Different Risks, Different Rules
Warfarin works differently than DOACs. It doesn’t depend on CYP3A4 or P-gp. Instead, it’s affected by vitamin K intake and other liver enzymes. That makes it less prone to some interactions - but not immune. Azvudine, an antiviral used in some countries, can raise INR levels, pushing patients into dangerous bleeding territory. One case study showed a patient’s INR jumping from 2.5 to 3.2 after adding azvudine and dexamethasone to his warfarin regimen.
But here’s the catch: warfarin requires constant monitoring. You need regular blood tests to check your INR. During the pandemic, many clinics shut down or cut back. A US Pharmacist report found that time spent in the safe INR range dropped by 18-22% during the peak months. That’s not just inconvenient - it’s dangerous. Without those checks, you’re flying blind.
DOACs don’t need routine blood tests, which made them popular. But when they interact with antivirals, you can’t rely on that convenience. There’s no easy way to know if your drug level is too high or too low unless you get specialized tests like anti-Xa levels - and most outpatient clinics don’t offer them.

Global Guidelines Don’t Agree - And That’s a Problem
There’s no global standard. The U.S. and Europe give conflicting advice on how to handle DOACs during Paxlovid treatment.
In the U.S., guidelines say: stop rivaroxaban and apixaban for the full 5-day Paxlovid course. Resume two days after. For dabigatran, if your kidney function is good (CrCl ≥50 mL/min), reduce the dose to 75 mg twice daily and take it at least 12 hours apart from Paxlovid. The European Medicines Agency, however, recommends cutting rivaroxaban’s dose by 50% instead of stopping it entirely.
Why the difference? It comes down to risk tolerance. The U.S. leans toward caution - better to pause the anticoagulant than risk bleeding. Europe tries to balance clotting risk, especially in high-risk patients. But for a patient with a CrCl of 40 mL/min - common in older adults - neither guideline gives clear direction. About 25% of elderly anticoagulated patients fall into this gray zone.
Real-World Chaos in Pharmacies and Clinics
Pharmacists were on the front lines. A survey by the American Pharmacists Association found that 63% of outpatient pharmacists saw at least one major anticoagulant interaction every month. Dabigatran and Paxlovid made up 42% of those cases.
At Mayo Clinic, anticoagulation-related ER visits jumped 37% in the first year of the pandemic. Nearly a third were directly tied to drug interactions. One Reddit user shared a harrowing story: a 68-year-old man on rivaroxaban took Paxlovid without telling his doctor. He ended up in the ICU with a GI bleed. He survived, but barely.
But there are success stories too. Dr. Sam Goldhaber shared a case where a high-risk patient with atrial fibrillation and prior clots was switched from rivaroxaban to daily enoxaparin injections during the Paxlovid course. After five days, they restarted the DOAC. No bleeding. No clots. It worked because the team planned ahead.

What You Should Do - Step by Step
If you’re on a blood thinner and get diagnosed with COVID-19, here’s what you need to do - right now:
- Don’t stop or change your dose on your own. Talk to your doctor or pharmacist immediately.
- Tell them exactly what you’re taking. Include supplements, over-the-counter painkillers, and herbal products. Many people don’t realize ibuprofen or St. John’s wort can also affect anticoagulants.
- Ask if you’re on a DOAC or warfarin. The advice changes completely based on which one.
- If you’re prescribed Paxlovid:
- For apixaban or rivaroxaban: Hold the dose for 5 days, restart 2 days after the last Paxlovid dose.
- For dabigatran: If your kidney function is normal, reduce to 75 mg twice daily and separate from Paxlovid by 12 hours. If your kidneys are impaired, hold it entirely and consider bridging with enoxaparin.
- For warfarin: Continue as usual, but check your INR every 2-3 days during treatment.
- Monitor for signs of bleeding: Unusual bruising, blood in stool or urine, severe headaches, vomiting blood. Call 911 if you suspect a major bleed.
- Watch for signs of clotting: Sudden shortness of breath, chest pain, swelling in one leg, numbness on one side of the face. These could mean a clot is forming.
The Future: Better Tools, Safer Drugs
The chaos we saw in 2020-2023 is slowly easing. Pfizer is developing a next-generation antiviral - PF-07817883 - that doesn’t inhibit CYP3A4. Early trials show it’s just as effective as Paxlovid but with far fewer drug interactions. It’s in Phase 2 as of mid-2023.
Meanwhile, AI is stepping in. A 2023 study in Nature Medicine built a machine learning model that predicts interaction severity with 89.4% accuracy using just 12 patient factors - age, kidney function, medication list, infection severity. Hospitals are starting to integrate this into their EHR systems.
And point-of-care testing is getting cheaper. Portable anti-Xa meters are now available for clinics, so you don’t need to wait days for lab results. If your DOAC level is too high, you can adjust immediately.
Still, the costs are rising. The Institute for Clinical and Economic Review estimates that managing these interactions will cost the U.S. $1.2 billion annually by 2025. That’s not just money - it’s ER visits, hospitalizations, lost workdays, and lives.
But here’s the good news: 87% of hematology experts surveyed by the American Society of Hematology believe these problems will be largely solved within the next 3-5 years. Better antivirals, smarter monitoring, and clearer guidelines are on the way.
For now, though, the message is simple: if you’re on a blood thinner and get sick with a respiratory infection, don’t assume your usual routine is safe. The interaction risks are real, unpredictable, and potentially deadly. Talk to your care team. Use the Liverpool COVID-19 Drug Interactions Checker. And never, ever change your meds without professional advice.
Can I take Paxlovid if I’m on a blood thinner?
Yes - but only under strict medical supervision. Paxlovid can dangerously increase levels of DOACs like apixaban, rivaroxaban, and dabigatran, raising bleeding risk. For apixaban and rivaroxaban, guidelines typically recommend stopping the anticoagulant during the 5-day Paxlovid course and restarting two days after. Dabigatran may be continued at a reduced dose with careful timing. Warfarin can usually be continued with closer INR monitoring. Never adjust your dose without consulting your doctor or pharmacist.
What are the signs that my blood thinner is interacting with COVID-19 meds?
If your anticoagulant level is too high, you may notice unusual bruising, nosebleeds, blood in urine or stool, vomiting blood, or severe headaches (possible brain bleed). If the level is too low - often due to dexamethasone - watch for sudden shortness of breath, chest pain, swelling or warmth in one leg (possible DVT), or numbness on one side of your body (possible stroke). These are medical emergencies.
Do I need blood tests while taking Paxlovid and a blood thinner?
If you’re on warfarin, yes - check your INR every 2-3 days during Paxlovid treatment. If you’re on a DOAC, routine blood tests aren’t standard, but anti-Xa levels can be ordered if your doctor suspects an interaction. These tests measure how much drug is in your blood and help determine if you’re under- or over-anticoagulated. Most clinics don’t offer them, so ask early.
Is it safer to switch from a DOAC to warfarin during COVID-19?
Not necessarily. Warfarin has fewer CYP3A4 interactions, but it requires frequent blood tests and is affected by diet and other drugs. Switching during an active infection adds complexity and risk - including the chance of clotting during the transition. Most experts recommend sticking with your current anticoagulant and adjusting the dose or timing instead, unless there’s a compelling reason to switch.
What if I can’t reach my doctor when I start Paxlovid?
Call your pharmacist. They have access to drug interaction databases like the Liverpool COVID-19 Drug Interactions Checker - which is updated daily and has handled over 1.2 million queries since 2020. Pharmacists are trained to spot these risks and can often advise you on temporary changes while you wait to speak with your doctor. Never guess - use the tools available.
How long should I stay on anticoagulants after recovering from COVID-19?
The American Society of Hematology recommends continuing therapeutic anticoagulation for at least 7 days after hospital discharge. For high-risk patients - those with prior clots, cancer, or severe illness - some experts extend this to 30-45 days. D-dimer levels often remain elevated for 14-21 days after recovery, so stopping too soon increases the risk of delayed clots. Your doctor should reassess your risk before stopping.

Olivia Hand
December 5, 2025 AT 23:43So let me get this straight - we’re giving people life-saving antivirals that can turn their blood into a ticking time bomb, and the solution is to stop their blood thinners and hope for the best? This isn’t medicine, it’s Russian roulette with a prescription pad.
Wesley Phillips
December 7, 2025 AT 03:45Wow. This post reads like a textbook chapter someone dumped into Reddit. I mean, the science is solid - but why not just say ‘don’t mix Paxlovid with DOACs without supervision’ and be done? You just gave me a 10-page pamphlet on why my grandma might bleed out. Thanks for the trauma.
Desmond Khoo
December 7, 2025 AT 17:29Y’all need to stop panicking and start talking to your pharmacist 😊 Seriously, they’re the real MVPs. I asked mine about my rivaroxaban + Paxlovid situation and she gave me a printed cheat sheet. No drama. Just clarity. 🙌
Louis Llaine
December 9, 2025 AT 15:27So the solution to a global health crisis is… more paperwork? Congrats, we turned a virus into a pharmacy exam. 🎓
Jane Quitain
December 11, 2025 AT 08:34i just got paxlovid and im on apixaban and i was so scared but then i called my dr and they told me to skip it for 5 days and restart after… i feel so much better now 😭 thank you for this post i wasnt sure what to do
Kyle Oksten
December 11, 2025 AT 22:29There’s a deeper issue here than drug interactions. We’ve built a system where patients are expected to navigate complex pharmacology on their own, while the medical infrastructure fails to keep pace. The real tragedy isn’t the bleeding - it’s that we accept this as normal.
Sam Mathew Cheriyan
December 12, 2025 AT 06:13fake news alert. paxlovid was made by big pharma to sell more blood thinners. the whole clotting thing is a scam to make people take more drugs. i read on a forum that covid is just a lab leak and the clots are from 5g towers. also, warfarin is cheaper so why not just use that? 🤔
Ernie Blevins
December 13, 2025 AT 02:15Everyone’s acting like this is new. It’s not. People die from drug interactions every day. This is just the latest headline. You think your doctor knows this stuff? Nah. They’re just reading the same pamphlets you are.
Nancy Carlsen
December 13, 2025 AT 21:25To anyone reading this and feeling overwhelmed - you’re not alone 💛 I’ve been on warfarin for 8 years and I’ve had panic attacks over this exact thing. But you’ve got this. Call your pharmacist. Write it down. Ask for help. You deserve to feel safe. 🌻
Ted Rosenwasser
December 14, 2025 AT 07:52Let’s be honest - if you’re taking DOACs and didn’t already know about CYP3A4 inhibition, you shouldn’t be on them. This isn’t a failure of the system - it’s a failure of patient education. I’ve seen patients on rivaroxaban who didn’t know what ‘anticoagulant’ meant. That’s not the drug’s fault. It’s yours.
Helen Maples
December 15, 2025 AT 07:46Step-by-step instructions? Excellent. But this post should have been published in JAMA, not Reddit. If you’re going to share life-saving information, do it with the rigor it deserves. No emojis. No fluff. Just facts. And citations. Always citations.
Ashley Farmer
December 15, 2025 AT 20:32I’m so glad someone wrote this. My mom had a stroke last year after stopping her DOAC too soon post-COVID. She didn’t know the risk lingered. This isn’t just info - it’s a lifeline. Thank you for taking the time to lay it out so clearly.
Wesley Phillips
December 17, 2025 AT 00:38Wow. You’re right - I didn’t even think about the lingering D-dimer risk. I just assumed once you’re out of the hospital, you’re fine. That Johns Hopkins stat? Chilling. I’m calling my doctor tomorrow to ask about my INR follow-up. Thanks, Olivia.