Azathioprine-Allopurinol Interaction Checker
This interactive tool helps you identify if you're taking a dangerous combination of azathioprine and allopurinol. This interaction can cause life-threatening bone marrow suppression.
Please note: This is for informational purposes only. Always consult your healthcare provider about your medications.
Combining allopurinol and azathioprine can be deadly-if you don’t know what you’re doing. This isn’t a theoretical risk. It’s a documented, life-threatening interaction that has sent patients to the ICU, caused severe bone marrow failure, and even led to death. And it’s happening more often than you think.
Why This Interaction Is So Dangerous
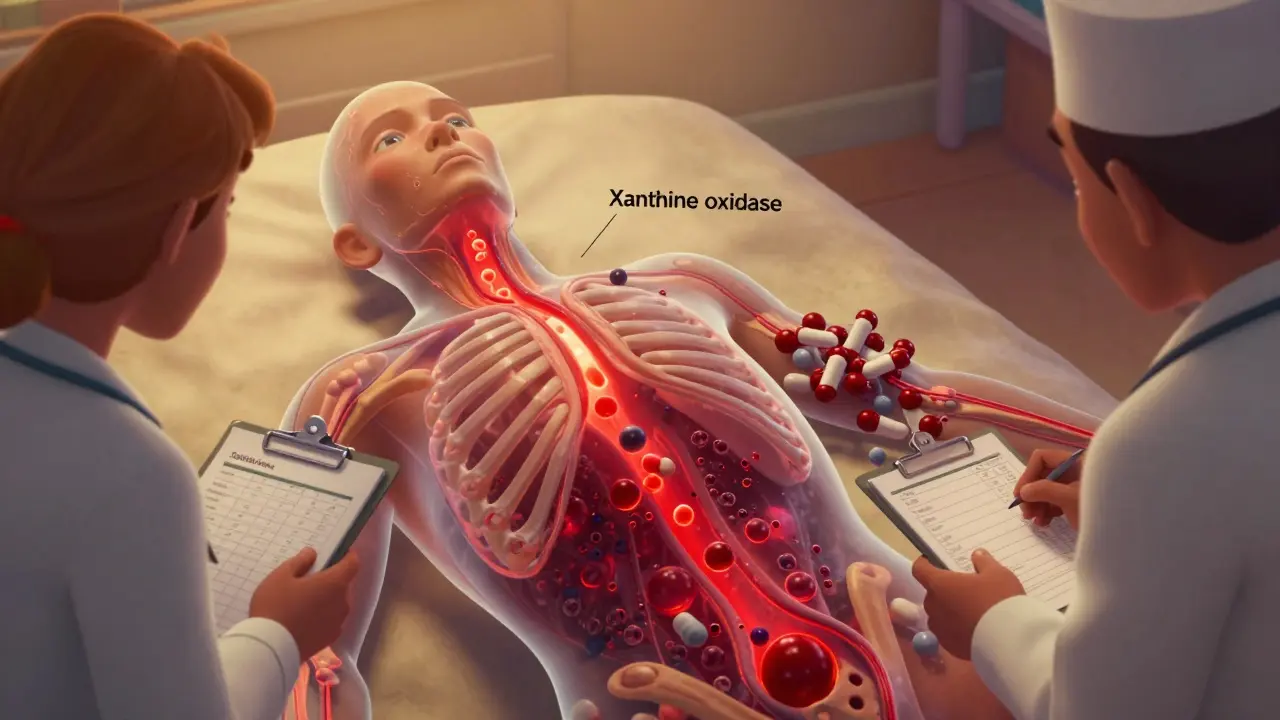
Allopurinol is a common gout medication. It lowers uric acid by blocking an enzyme called xanthine oxidase. Azathioprine is an immunosuppressant used for Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and after organ transplants. On paper, they seem unrelated. But inside your body, they collide in a way that can shut down your blood cell production. Here’s how: Azathioprine breaks down into 6-mercaptopurine (6-MP), the active ingredient that suppresses the immune system. Normally, xanthine oxidase helps clear 6-MP by turning it into harmless waste. But allopurinol blocks that enzyme. So instead of being safely removed, 6-MP builds up-sometimes to four times its normal level. That extra 6-MP gets converted into thioguanine nucleotides (6-TGNs), which flood into your bone marrow and destroy white blood cells, red blood cells, and platelets. The result? Pancytopenia. That means your blood counts crash. White blood cells drop below 1,000 per mm³ (normal is 4,000-11,000). Neutrophils-the cells that fight infection-can fall below 500. Platelets may drop below 20,000, turning even a minor cut into a bleeding emergency. Hemoglobin can plunge to 3.7 g/dL. At that level, you’re barely carrying oxygen. One case from 1996 showed a patient needing four blood transfusions and a costly hospital stay that would cost over $25,000 today.The Black Box Warning You Might Not Know About
The FDA requires azathioprine (brand name Imuran) to carry a black box warning-the strongest safety alert they issue. It says clearly: “Concomitant use of allopurinol and azathioprine increases the risk of life-threatening bone marrow suppression.” Yet, this warning still gets missed. Why? Because gout and inflammatory bowel disease often overlap. A 63-year-old man with a kidney transplant takes azathioprine. He gets wrist pain. His doctor assumes it’s gout and prescribes allopurinol. No one checks his meds. No one thinks to ask if he’s on an immunosuppressant. That’s exactly what happened in the landmark 1996 case that first brought this interaction to light. The patient survived-but barely. Since then, dozens of similar cases have been reported. A 57-year-old man in 2021 developed severe myelosuppression after starting allopurinol for gout while on azathioprine for Crohn’s. He was hospitalized for weeks. His doctors had no idea the two drugs were interacting.When Is It Safe to Use Them Together?
There’s one exception-and it’s not for everyone. Some patients with inflammatory bowel disease are called “thiopurine shunters.” Their bodies convert too much azathioprine into a toxic metabolite called 6-MMP instead of the therapeutic 6-TGN. This causes liver damage, not bone marrow failure. For these patients, adding a low dose of allopurinol can redirect metabolism toward 6-TGN and away from 6-MMP. In a 2018 study, 53% of IBD patients on this combo went into steroid-free remission. That’s huge. But here’s the catch: This is not a DIY treatment. It requires expert management. The protocol is strict:- Azathioprine dose must be cut to 25% of normal (0.5-0.75 mg/kg/day instead of 2-2.5 mg/kg/day)
- Allopurinol is started at 100 mg daily
- Complete blood counts must be checked weekly for the first month, then every two weeks for two months, then monthly
- Thiopurine metabolite levels (6-TGN and 6-MMP) must be monitored
- Therapeutic 6-TGN range: 230-450 pmol/8×10⁸ RBCs
- 6-MMP must stay below 5,700 pmol/8×10⁸ RBCs
What Happens If You Ignore the Rules?
If you don’t reduce the azathioprine dose, you’re playing Russian roulette with your bone marrow. A 2022 review documented cases where patients developed full-blown pancytopenia within weeks. One patient’s white blood cell count dropped to 1.1 × 10³/mm³. Another’s platelets fell to 18,000. Both needed intensive care, growth factor injections, and blood transfusions. Even when doses are adjusted, the risk doesn’t disappear. Some patients still develop toxicity. That’s why monitoring isn’t optional-it’s mandatory. Skipping a blood test for a month can mean the difference between catching a problem early and losing your life to an infection you can’t fight.Who’s at Highest Risk?
Not everyone reacts the same way. Genetics play a big role. About 10% of people have intermediate activity of an enzyme called TPMT (thiopurine methyltransferase). This enzyme helps break down 6-MP. If you have low or intermediate TPMT activity, even standard doses of azathioprine can be dangerous. Add allopurinol, and the risk skyrockets. Also, older adults, people with kidney disease, and those already on other bone marrow-suppressing drugs (like methotrexate or cyclophosphamide) are at higher risk. If you’re on azathioprine and your doctor suggests allopurinol for gout, ask: “Have you checked my TPMT status? Have you looked at my current metabolite levels?”
What Are the Alternatives?
If you’re on azathioprine and need gout treatment, there are safer options:- Febuxostat: Another xanthine oxidase inhibitor, but it doesn’t interact with azathioprine the same way. It’s often the preferred alternative.
- Pegloticase: Used for severe, treatment-resistant gout. Given by IV, it breaks down uric acid directly.
- Colchicine: For acute gout flares, not long-term prevention, but it doesn’t affect azathioprine metabolism.
- Nonsteroidal anti-inflammatories (NSAIDs): Can help with pain during flares, but avoid if you have kidney issues.
What Should You Do?
If you’re taking azathioprine:- Never start allopurinol without talking to your specialist
- Carry a list of all your medications-especially immunosuppressants
- Ask your pharmacist to review your entire drug list
- Know the signs of bone marrow suppression: fever, fatigue, bruising, bleeding gums, frequent infections
- If you feel unwell after starting a new drug, get a blood test immediately
- Ask: “Am I on any immunosuppressants?”
- If yes, tell your doctor immediately
- Don’t assume your rheumatologist knows what your gastroenterologist prescribed
Bottom Line
Allopurinol and azathioprine together are not just risky-they’re potentially lethal. Most doctors know this. But not all. And patients? Most have never heard of this interaction. The good news? With proper monitoring and expert care, this combo can help a small group of patients with stubborn IBD. The bad news? It’s a high-wire act. One misstep, and you’re falling. If you’re on either drug, don’t wait for a crisis. Talk to your doctor now. Ask for a full medication review. Get your blood counts checked. Know your options. Your life might depend on it.Can I take allopurinol if I’m on azathioprine?
Generally, no. Combining allopurinol and azathioprine can cause life-threatening bone marrow suppression. The only exception is in specialized IBD care, where low-dose allopurinol is used under strict monitoring to redirect azathioprine metabolism. This should only be done by experts with access to blood metabolite testing and weekly blood counts.
What are the signs of azathioprine and allopurinol toxicity?
Watch for fever, extreme fatigue, unexplained bruising or bleeding, frequent infections, pale skin, shortness of breath, or a rapid heartbeat. These can signal low white blood cells, red blood cells, or platelets. If you’re on both drugs and experience any of these, get a complete blood count immediately. Don’t wait.
Is febuxostat safer than allopurinol if I’m on azathioprine?
Yes. Febuxostat is a different type of xanthine oxidase inhibitor that does not significantly interfere with azathioprine metabolism. It’s the preferred alternative for gout treatment in patients taking azathioprine. Always confirm with your doctor before switching, but febuxostat avoids the dangerous interaction seen with allopurinol.
How often should blood tests be done if I’m on both drugs?
If the combination is absolutely necessary (only in specialized IBD care), blood counts must be checked weekly for the first month, then every two weeks for two months, then monthly. Thiopurine metabolite levels (6-TGN and 6-MMP) should also be tested before starting and every 3-6 months. Skipping tests increases the risk of fatal toxicity.
Can my pharmacist help me avoid this interaction?
Absolutely. Pharmacists are trained to spot dangerous drug interactions. When you pick up azathioprine or allopurinol, ask your pharmacist to run a full drug interaction check. Many pharmacies now flag this combination automatically. If they don’t, ask why. This is a black box warning for a reason.

