What if you could fix your insomnia without popping a pill every night? No grogginess. No dependency. No morning fog. Just better sleep-naturally. That’s not a fantasy. It’s CBT-I-Cognitive Behavioral Therapy for Insomnia-and it’s the most effective, science-backed way to reclaim your nights.
Why Pills Don’t Solve Insomnia
Sleeping pills might help you drift off the first night. But after that? They lose their power. Studies show that after a few weeks, your body builds tolerance. You need more to get the same effect. And when you stop? Your insomnia often comes back worse than before. The American College of Physicians says it plainly: for chronic insomnia, CBT-I should be your first move-not your last resort. Why? Because pills only mask the problem. CBT-I fixes the root cause. Think of it like this: if your car won’t start because the battery is dead, you don’t just keep pushing it. You fix the battery. Insomnia isn’t about being too tired to sleep. It’s about your brain and body having learned the wrong habits. CBT-I rewires those habits.What Is CBT-I? (And Why It’s Not Just ‘Good Sleep Hygiene’)
You’ve probably heard the advice: “No caffeine after noon,” “Keep your bedroom cool,” “Put your phone away.” Those are sleep hygiene tips. Helpful? Sure. But they’re not enough for chronic insomnia. CBT-I is a structured, step-by-step program backed by over 40 years of research. It’s not a one-size-fits-all checklist. It’s a personalized toolkit that targets the thoughts and behaviors keeping you awake. Developed by sleep scientists like Dr. Arthur Spielman and Dr. Jack Edinger, it’s been tested in thousands of people-and it works. The Sleep Foundation says 70% to 80% of people with primary insomnia see major improvement after CBT-I. And unlike pills, the gains stick. A 2023 study in JAMA Network Open found that 76% of people using digital CBT-I still had better sleep six months later. That’s not luck. That’s learning.The Five Core Techniques of CBT-I
CBT-I isn’t one trick. It’s five proven strategies working together. You don’t need to do them all at once. But skipping any of them reduces your chances of long-term success.1. Stimulus Control Therapy
Your bed should be for sleep-and sex-only. Not scrolling. Not worrying. Not watching TV. If you’ve been lying awake for more than 20 minutes, get up. Go to another room. Do something quiet and dimly lit-read a book, listen to calm music. Don’t check the clock. Come back to bed only when you feel sleepy. This breaks the mental link between your bed and frustration. Over time, your brain starts to associate your bed with sleep, not stress.2. Sleep Restriction Therapy
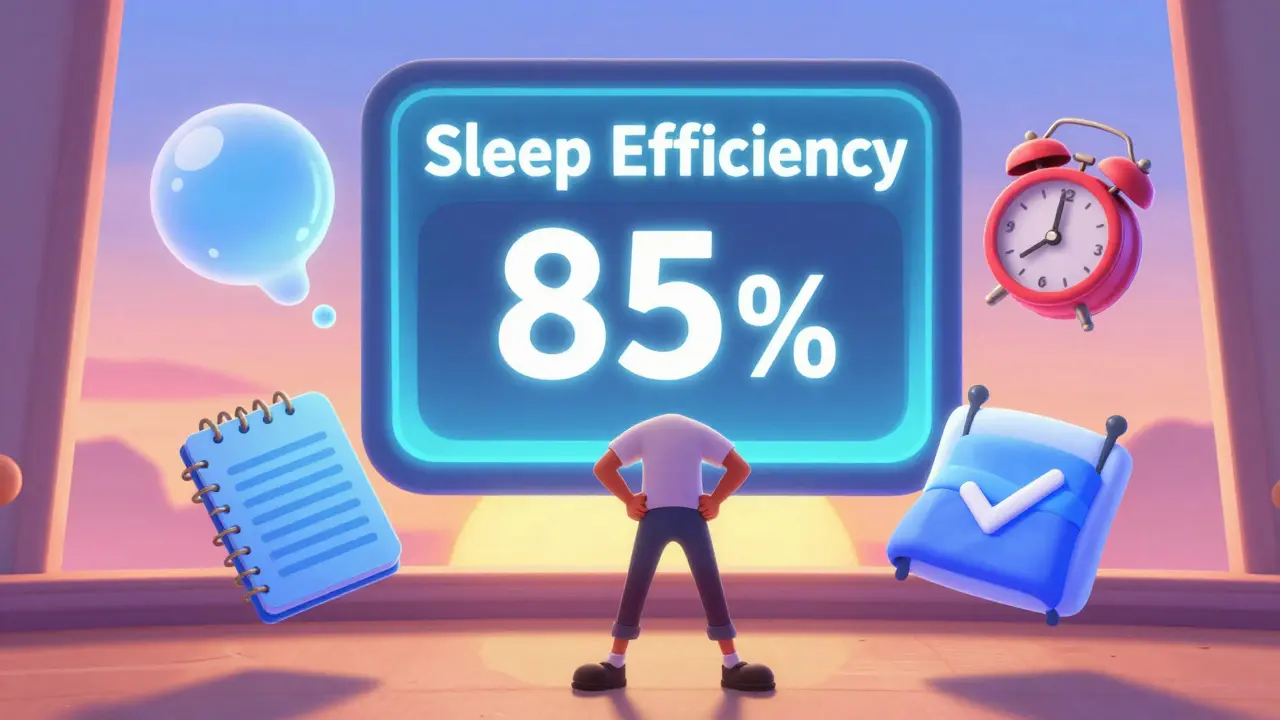
This one sounds counterintuitive. And yes, it’s hard at first. You calculate your average total sleep time over the past week. If you’re only sleeping 5 hours a night, you limit your time in bed to 5 hours. That might mean going to bed at 1 a.m. and waking at 6 a.m.-even if you’re tired. Why? You’re building sleep pressure. The more sleep-deprived you are (temporarily), the harder your body works to fall asleep. It’s like resetting a muscle that’s gone weak from underuse. Most people feel exhausted for the first 3-7 days. But after that, sleep efficiency shoots up. You’re not just spending more time in bed-you’re actually sleeping more of it. The goal? Reach 85% sleep efficiency. That means if you’re in bed for 7 hours, you’re sleeping at least 6 hours.3. Cognitive Restructuring
Your thoughts about sleep are sabotaging you. “I’ll be useless tomorrow if I don’t sleep 8 hours.” “If I don’t fall asleep in 10 minutes, something’s wrong.” “I’ve been this way for years-this is just who I am.” These aren’t facts. They’re fears dressed up as truth. CBT-I teaches you to challenge them. Ask yourself: “What’s the evidence this thought is true?” “What’s a more realistic way to see this?” “What would I tell a friend who said this?” One study found that people who changed their sleep-related beliefs improved their sleep more than those who just followed behavioral tips. Your mind is your biggest sleep obstacle-and your greatest ally.4. Sleep Hygiene (The Right Way)
This isn’t just “avoid coffee.” It’s about creating a sleep-friendly environment and routine.- Keep your bedroom cool (around 18-19°C), dark, and quiet.
- Use your bed only for sleep and intimacy-no work, no phones.
- Get natural light in the morning. Even 15 minutes helps reset your clock.
- Limit alcohol. It might make you drowsy, but it ruins deep sleep.
- Avoid heavy meals or intense exercise 2-3 hours before bed.
5. Relaxation Training
Your body is stuck in “alert” mode. Even when you’re lying still, your nervous system is racing. CBT-I teaches you how to turn it down. Two techniques work best:- Diaphragmatic breathing: Breathe in slowly through your nose for 4 counts, hold for 4, exhale through your mouth for 6. Repeat for 5 minutes. This signals safety to your brain.
- Progressive muscle relaxation: Tense each muscle group (toes → feet → calves → thighs → etc.) for 5 seconds, then release. Notice the difference between tension and calm.
How Long Does It Take?
Most people see changes in 2-4 weeks. But full results take 6-8 weeks. The first week is the toughest. Sleep restriction means less sleep. You’ll feel tired. That’s normal. Your body is adjusting. By week 3, most people report falling asleep faster. By week 6, they’re waking up less. And by week 8? Many say they’ve forgotten what it’s like to lie awake for hours. A 2015 meta-analysis of 20 studies found CBT-I reduced the time it took to fall asleep by 19 minutes and cut nighttime awakenings by 26 minutes. That’s more than an hour of extra sleep per night-without a single pill.
Digital CBT-I: The Easiest Way to Start
Finding a trained CBT-I therapist can be hard. In the U.S., there are only about 1,500 certified specialists for 330 million people. That’s why digital CBT-I is exploding. Apps like Sleepio and CBT-i Coach deliver the full program through your phone or tablet. They guide you through daily exercises, track your sleep diary, and adjust your plan based on your progress. The 2023 JAMA Network Open study showed digital CBT-I worked just as well as in-person therapy. In fact, 77% of users responded positively after just one month. And 76% still had better sleep six months later. Medicare and 85% of private insurers now cover digital CBT-I. Some employers offer it for free through wellness programs. Check your benefits.Who Can Benefit?
CBT-I isn’t just for adults. A 2024 study in Frontiers in Public Health found it worked just as well for teens. No pills. No side effects. Just better sleep. It’s also safe and effective for:- Pregnant people (medications can be risky)
- People with PTSD or anxiety
- Cancer survivors
- Older adults
What to Expect When You Start
You’ll need a sleep diary. Write down:- Bedtime
- Time you actually fell asleep
- Number of awakenings
- Wake-up time
- How rested you felt
Common Mistakes (And How to Avoid Them)
- Mistake: Giving up after a bad night. Fix: One bad night doesn’t undo progress. Keep going.
- Mistake: Trying to sleep. Fix: Don’t fight sleep. Just lie quietly. Let it come.
- Mistake: Checking the clock. Fix: Put your phone and clock out of sight. Time anxiety keeps you awake.
- Mistake: Comparing yourself to others. Fix: Your sleep is your own. Progress isn’t linear.
Why CBT-I Beats Pills in the Long Run
Pills give you a quick fix. CBT-I gives you a lifelong skill. At six months, people using CBT-I still had 12.4% higher sleep efficiency than those on medication. They slept more deeply. Woke up less. Felt more alert during the day. And they didn’t need to keep taking anything. Medication side effects? Dizziness, memory issues, dependency. CBT-I? None. No withdrawal. No rebound insomnia. Dr. Donn Posner from the Mayo Clinic says it best: “Unlike sleeping pills, CBT helps you overcome the causes of your sleep problems.” You’re not just sleeping better. You’re learning how to sleep-naturally, reliably, for life.Ready to Try It?
Start today:- Download a free sleep diary app (or use a notebook).
- Track your sleep for 7 days.
- Set a fixed wake-up time-even on weekends.
- Leave your bed if you’re awake for more than 20 minutes.
- Try 5 minutes of diaphragmatic breathing before bed.
Can CBT-I really work if I’ve had insomnia for years?
Yes. CBT-I works even for people who’ve struggled with insomnia for decades. Research shows that long-term insomnia is often maintained by learned behaviors and negative thoughts-not a physical inability to sleep. CBT-I breaks those patterns. A 2023 study found that people with 10+ years of insomnia still had a 72% improvement rate after completing a full CBT-I program. The longer you’ve had it, the more your brain needs to relearn, but the results are just as lasting.
Will I feel worse before I feel better?
It’s common, especially during the first week of sleep restriction. You might be sleeping 30-60 minutes less than usual. That can make you tired, irritable, or foggy during the day. But this is temporary. Your body is recalibrating. Most people report feeling significantly better by day 7-10. The fatigue isn’t a sign it’s not working-it’s part of the process. Stick with it.
Do I need to stop taking sleeping pills to do CBT-I?
Not necessarily. Many people start CBT-I while still on medication. The goal isn’t to quit cold turkey-it’s to reduce reliance over time. Your therapist or digital program will help you taper off safely, usually after you’ve improved your sleep efficiency and feel more confident in your ability to sleep without pills. Never stop medication abruptly without medical advice.
Is CBT-I covered by insurance?
Yes, increasingly so. Since the American College of Physicians recommended CBT-I as first-line treatment in 2016, Medicare and 85% of large private insurers now cover both in-person and digital CBT-I. Check with your provider. Some employers offer it as part of wellness programs. Digital options like Sleepio and CBT-i Coach often have direct insurance billing or are available at low cost through workplace health plans.
What if I can’t stick to the schedule?
Consistency matters, but perfection isn’t required. If you sleep in on Saturday, aim to keep it within 30-60 minutes of your usual wake time. If you nap, try to skip it the next day. The key is to keep returning to the routine. Most people slip up early on. The ones who succeed are the ones who don’t give up after one bad day. Progress, not perfection, is the goal.
Can CBT-I help with waking up too early?
Yes. Early waking is often linked to being in bed too long or having a misaligned circadian rhythm. CBT-I addresses this through sleep restriction (limiting time in bed to match actual sleep) and strict wake times. By consolidating sleep into a shorter window, you reduce the chance of waking up too early. Light exposure in the morning also helps reset your internal clock. Many people who wake at 4 a.m. find they’re sleeping through until 6 a.m. after 4-6 weeks of CBT-I.
How do I know if I have chronic insomnia?
Chronic insomnia means you have trouble falling asleep, staying asleep, or waking up too early-at least three nights a week for three months or longer. It also causes daytime problems like fatigue, trouble focusing, or mood issues. If you’ve been struggling this long and it’s affecting your life, CBT-I is the most effective next step. Short-term insomnia (under 3 months) often resolves on its own, but chronic insomnia needs a structured approach.


Alexandra Enns
January 24, 2026 AT 05:12Also, digital apps? Please. My great-grandma slept better with a hot toddy and a prayer.
Marie-Pier D.
January 24, 2026 AT 15:26You're not just teaching sleep-you're giving people their lives back. 💙
Shanta Blank
January 25, 2026 AT 07:08CBT-I doesn't 'work.' It's just the pharmaceutical industry's way of offloading their failed drug empire onto your mental health. You think they want you to fix your sleep? No. They want you to buy their $99/month app subscription so they can sell your data to advertisers.
Meanwhile, I take 2 mg of melatonin and nap like a boss. Sleep is a privilege, not a project.
Chloe Hadland
January 25, 2026 AT 16:33but then yesterday i fell asleep before my head hit the pillow and i didn't even realize it. it felt like magic.
still not perfect but i'm not panicking anymore when i wake up at 2am. that's huge for me
Amelia Williams
January 26, 2026 AT 11:32My boss noticed I’m not snapping at people. My partner says I smell less like anxiety. My cat sleeps on my chest again.
This isn’t a cure-it’s a homecoming. And it’s free. No pills. No gimmicks. Just you, your bed, and the quiet courage to stop fighting.