One in three women over 50 will break a bone because of weak bones. One in five men will too. And most of them had no idea their bones were crumbling until it was too late. This isn’t just about getting older. It’s about what you’ve been doing - or not doing - for years. Bone loss doesn’t come with pain. It doesn’t show up on a scan until it’s already serious. But it’s not inevitable. You can stop it. You can even rebuild a little. And the time to start isn’t when you fall. It’s now.
Why Your Bones Are Weakening (And Why It’s Silent)
Your bones aren’t static. They’re alive, constantly breaking down old tissue and building new. Up until your mid-20s, you’re building more than you lose. That’s your peak bone mass. After that, the scale tips. You lose about 0.3% to 0.5% a year. For men, that’s slow. For women, after menopause, it spikes to 2-3% a year for five to seven years. That’s like losing a quarter of your bone strength in just five years.
This isn’t about calcium alone. It’s about balance. When your body breaks down bone faster than it rebuilds it, you get osteoporosis. And here’s the problem: you won’t feel it. No aches. No warning. Just a fracture - often from a fall that shouldn’t have hurt, like stepping off a curb or sneezing too hard.
By the time you break a bone, your bone density might already be 30% lower than it was at 30. And once you’ve had one fracture, your risk of another jumps by up to 200%. That’s not bad luck. That’s biology.
What You Can’t Change - And What You Can
Some risks are fixed. You can’t undo your age. You can’t change your gender. If you’re a woman of White or Asian descent, your risk is higher than for Black or Hispanic women. If your mom broke a hip, your risk goes up by 60-80%. Early menopause? That’s another red flag.
But here’s the good news: most of what drives osteoporosis is in your control.
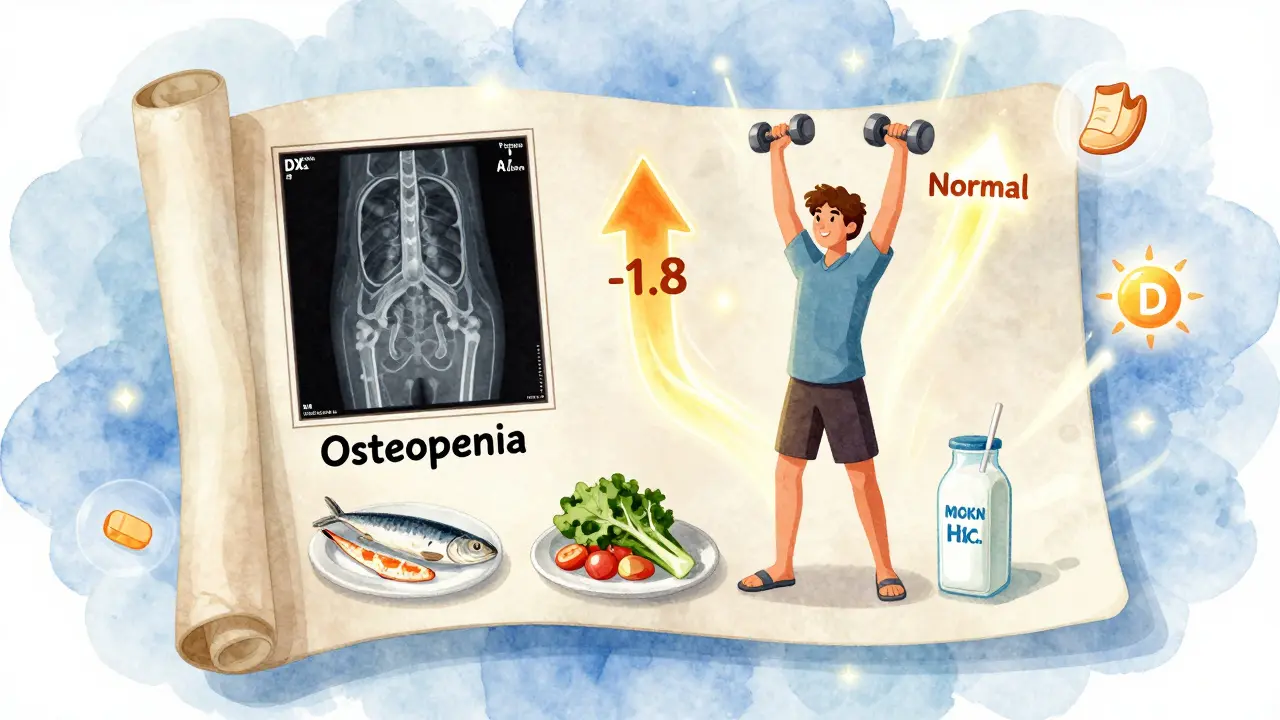
- Calcium intake: If you’re not getting 1,000-1,200 mg a day, you’re falling behind. That’s not one glass of milk. That’s three servings of dairy - or equivalent amounts of fortified plant milk, tofu, kale, or sardines with bones. Most people fall short by 400-600 mg daily.
- Vitamin D: If your blood level is below 20 ng/mL (and 42% of U.S. adults are), your fracture risk jumps 33%. You need 800-1,000 IU a day. If you’re deficient, you might need 2,000 IU for a few months to catch up.
- Smoking: One pack a day increases your risk by 55%. It messes with calcium absorption and lowers estrogen - the hormone that protects your bones.
- Alcohol: More than two drinks a day? That’s a 41% higher chance of a hip fracture. It’s not just the calories. Alcohol kills bone-building cells.
- Sitting: If you’re inactive, your fracture risk is 25-30% higher. Movement tells your bones to stay strong. No movement? They think they’re not needed - and start to disappear.
These aren’t guesses. These are numbers from large studies tracking hundreds of thousands of people. And they’re not just for older adults. The habits you build at 40 shape your bones at 70.
The Exercise That Actually Builds Bone
Walking helps. But it’s not enough. To build bone, you need impact and resistance.
Brisk walking, jogging, stair climbing, dancing - these are weight-bearing exercises. They force your bones to support your body’s weight. That stress tells your body: "Keep this bone strong."
Then add resistance. Lifting weights, using resistance bands, doing squats or push-ups - even if it’s light. Two days a week is the minimum. You don’t need to bench press. You need to challenge your muscles and bones.
A 2023 Yale study followed 2,543 people over 60. Those who did 30 minutes of weight-bearing exercise five days a week and strength training twice a week reduced their fracture risk by 30-40%. And after six months, they didn’t just have stronger bones - they had better balance. Fewer falls. Fewer fractures.
And here’s the kicker: you don’t need a gym. You can do bodyweight squats at home. Walk up and down stairs. Carry groceries. Stand on one foot while brushing your teeth. It’s not about intensity. It’s about consistency.

Medications - When They Help, When They Don’t
If your bone density is already low (T-score below -2.5), or you’ve had a fracture, your doctor might recommend medication. Bisphosphonates like alendronate or risedronate are common. They slow bone loss. But they’re not magic.
On Reddit’s osteoporosis community, 75% of users report side effects - stomach pain, muscle aches, jaw issues. And 38% stop taking them within a year. That’s dangerous. Stopping means the bone loss resumes.
Newer drugs like romosozumab (Evenity) actually build new bone - not just slow loss. But they’re expensive and only used for a year, then switched to another drug. They’re not for everyone.
The key? Don’t rely on pills alone. Medication works best when paired with calcium, vitamin D, and exercise. Take the pill and sit on the couch? You’re wasting your time.
Testing: What the Numbers Really Mean
A DXA scan is the gold standard. It’s quick - 15-20 minutes. The radiation? Less than a flight from Durban to Cape Town. It measures bone density in your hip and spine. Results come as a T-score:
- Normal: -1.0 or higher
- Osteopenia: -1.0 to -2.5 (low bone mass)
- Osteoporosis: -2.5 or lower
But here’s what most people don’t know: up to half of people who break bones have T-scores in the osteopenia range - not osteoporosis. That’s why doctors now use the FRAX tool. It doesn’t just look at bone density. It adds your age, sex, weight, smoking status, alcohol use, and whether you’ve had a prior fracture.
Dr. Ethel Siris says it best: "A single fragility fracture doubles your risk of another. That’s more important than any scan." If you’ve broken a bone after 50 from a minor fall, you already have osteoporosis - even if your scan says otherwise.
Fall Prevention: The Hidden Key
Weak bones are only half the problem. The other half? Falling.
Most fractures happen at home. Loose rugs. Poor lighting. Cluttered hallways. No handrails on stairs. Slippery bathroom floors.
Simple fixes work:
- Install grab bars in the shower and next to the toilet
- Remove throw rugs or tape them down
- Use nightlights in hallways and bathrooms
- Keep frequently used items on middle shelves
- Wear shoes with non-slip soles - no socks on hardwood
Balance training helps too. Stand on one foot while brushing your teeth. Walk heel-to-toe. Do tai chi. These aren’t exercises for yoga studios. They’re survival skills.
The CDC’s STEADI program shows these changes reduce falls by nearly 30% in a year. That’s 30% fewer fractures. That’s 30% fewer hospital visits. That’s 30% fewer lost months of independence.
What You Should Do Right Now
Here’s your action plan - no doctor’s visit required yet:
- Check your calcium and vitamin D. Are you getting 1,000-1,200 mg of calcium daily? Are you taking 800-1,000 IU of vitamin D? If not, start today.
- Move every day. Walk for 30 minutes. Lift something heavy - even a bag of rice. Do two strength sessions a week. No gym? Use your body.
- Quit smoking. If you smoke, stop. If you don’t, don’t start.
- Limit alcohol. Stick to one drink a day. Two is too much.
- Make your home safer. Look around your house. What could cause a fall? Fix it.
- Ask for a bone scan. If you’re a woman over 65, or a man over 70 - or if you’re over 50 and have risk factors (family history, low body weight, steroid use), ask your doctor about a DXA scan.
This isn’t about fear. It’s about control. Your bones are your foundation. They hold you up. They let you move. They let you live. And they’ve been listening to everything you’ve done - or not done - for decades.
It’s not too late to change the story.
Can osteoporosis be reversed?
You can’t fully restore bone density to what it was at 25, but you can stop the loss - and even rebuild a little. Weight-bearing exercise, adequate calcium and vitamin D, and certain medications can increase bone density by 1-3% per year. That’s enough to significantly lower fracture risk. The goal isn’t perfection. It’s protection.
Do I need a bone density scan if I’m under 50?
Usually not - unless you have risk factors. If you’ve had a fracture after age 45, take long-term steroids, have rheumatoid arthritis, type 1 diabetes, or an early menopause, or have a parent who broke a hip, talk to your doctor. Early detection can change outcomes.
Is milk the best source of calcium?
Milk is convenient, but not the only option. Fortified plant milks, canned sardines with bones, tofu made with calcium sulfate, kale, broccoli, and almonds all provide calcium. The key is consistency - not the source. You need 1,000-1,200 mg daily, no matter where it comes from.
Can supplements cause side effects?
Yes. Calcium supplements can cause constipation or bloating. Taking them with food helps. Vitamin D is generally safe, but high doses (over 4,000 IU daily long-term) can raise calcium levels too much. Stick to recommended doses unless your doctor says otherwise. If you have kidney stones or kidney disease, talk to your doctor before starting supplements.
How long until I see results from exercise?
Bone changes slowly. You won’t feel it. But after 6-12 months of consistent weight-bearing and strength training, scans show measurable improvements. The real win? Better balance, less fear of falling, and more confidence to move - that happens much sooner.
Is osteoporosis only a women’s issue?
No. While women are four times more likely to develop it, men over 50 have a 1 in 5 chance of breaking a bone due to osteoporosis. Men are also more likely to die after a hip fracture. But men are less likely to get tested or treated. Bone health matters for everyone.

